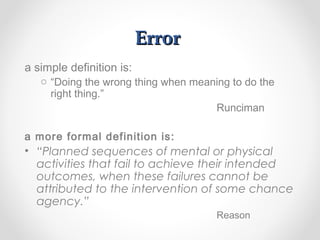
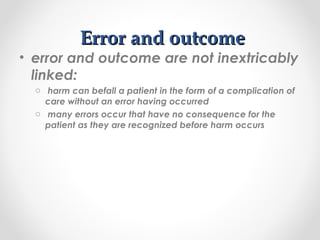
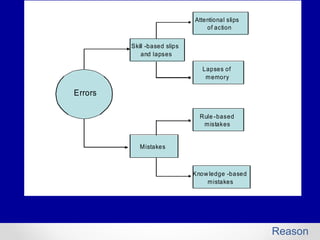
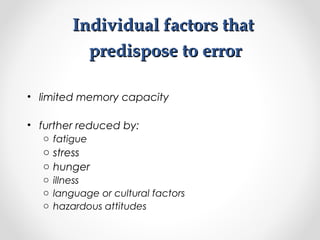
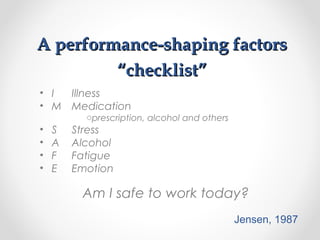
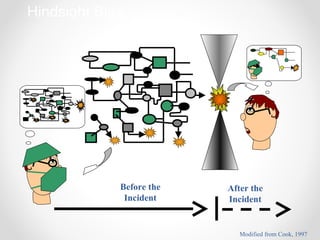
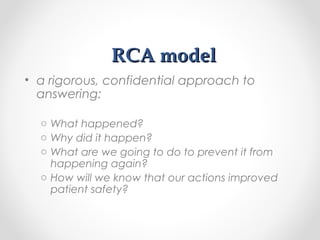
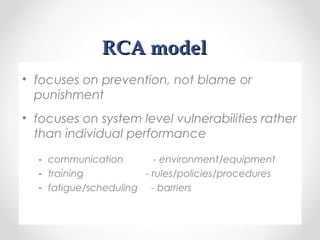
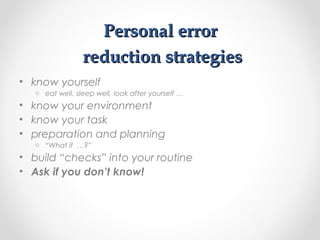
This document discusses medical error and strategies for learning from errors to improve patient safety. It defines key terms like error, violation, and near miss. It explains that errors are an inevitable human factor and discusses individual and situational factors that can increase error risk. The document advocates for a non-punitive culture where errors are reported anonymously so their root causes can be analyzed systematically to design error-proofing strategies and remove "error traps" from the system.