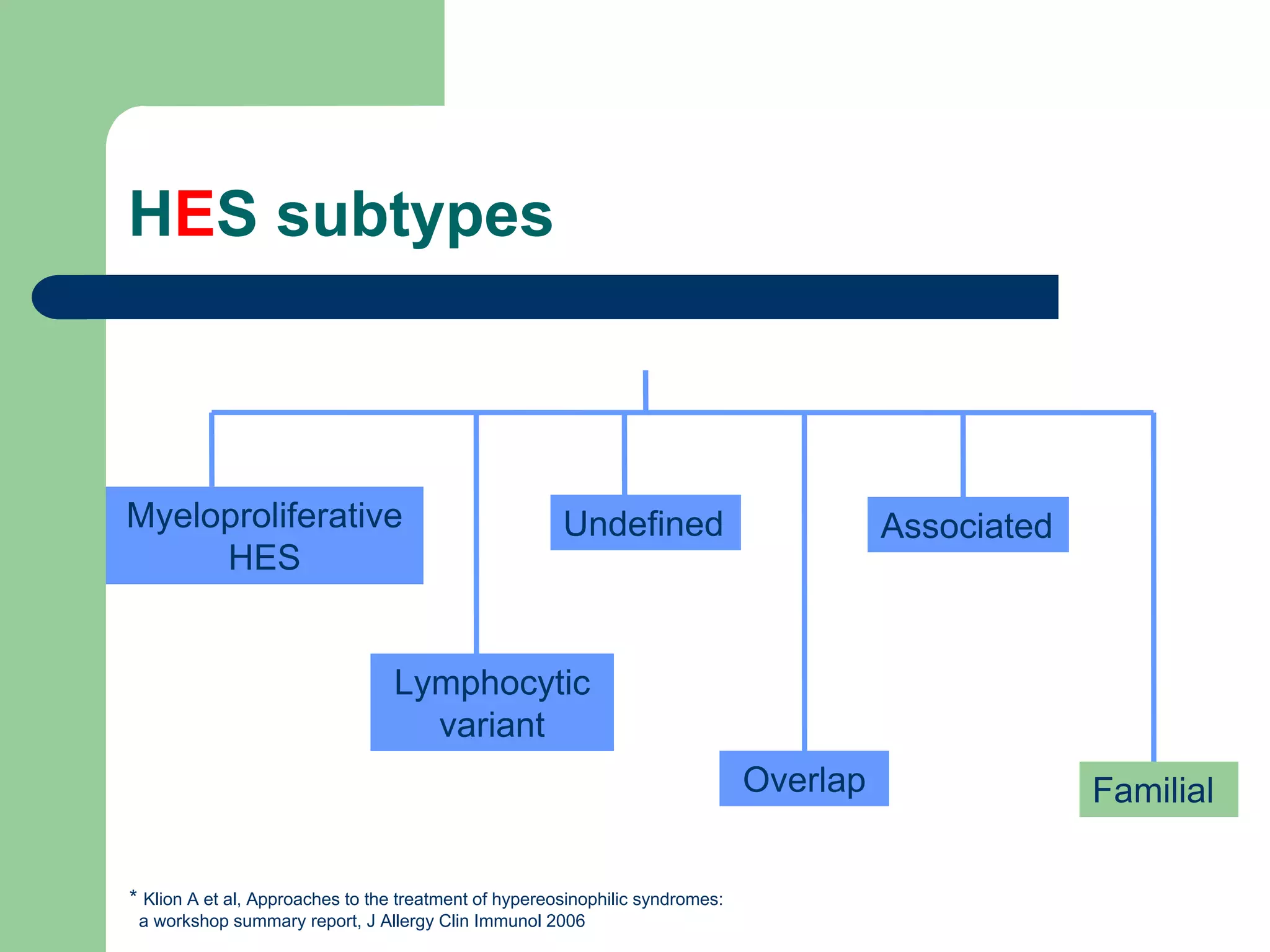
This document discusses eosinophils and eosinophilia. It begins with two case studies, one involving a 57-year-old man with a history of asthma and eosinophilia, and another involving a 28-year-old man diagnosed with hypereosinophilic syndrome after presenting with heart failure and marked eosinophilia. It then provides information on what eosinophils are, their role in the immune system, common causes of eosinophilia including allergies, parasites, and certain drugs. It discusses different subtypes of hypereosinophilic syndrome and their treatment options. It concludes by explaining how eosinophil activation can lead to tissue damage in some individuals with eosinophilia