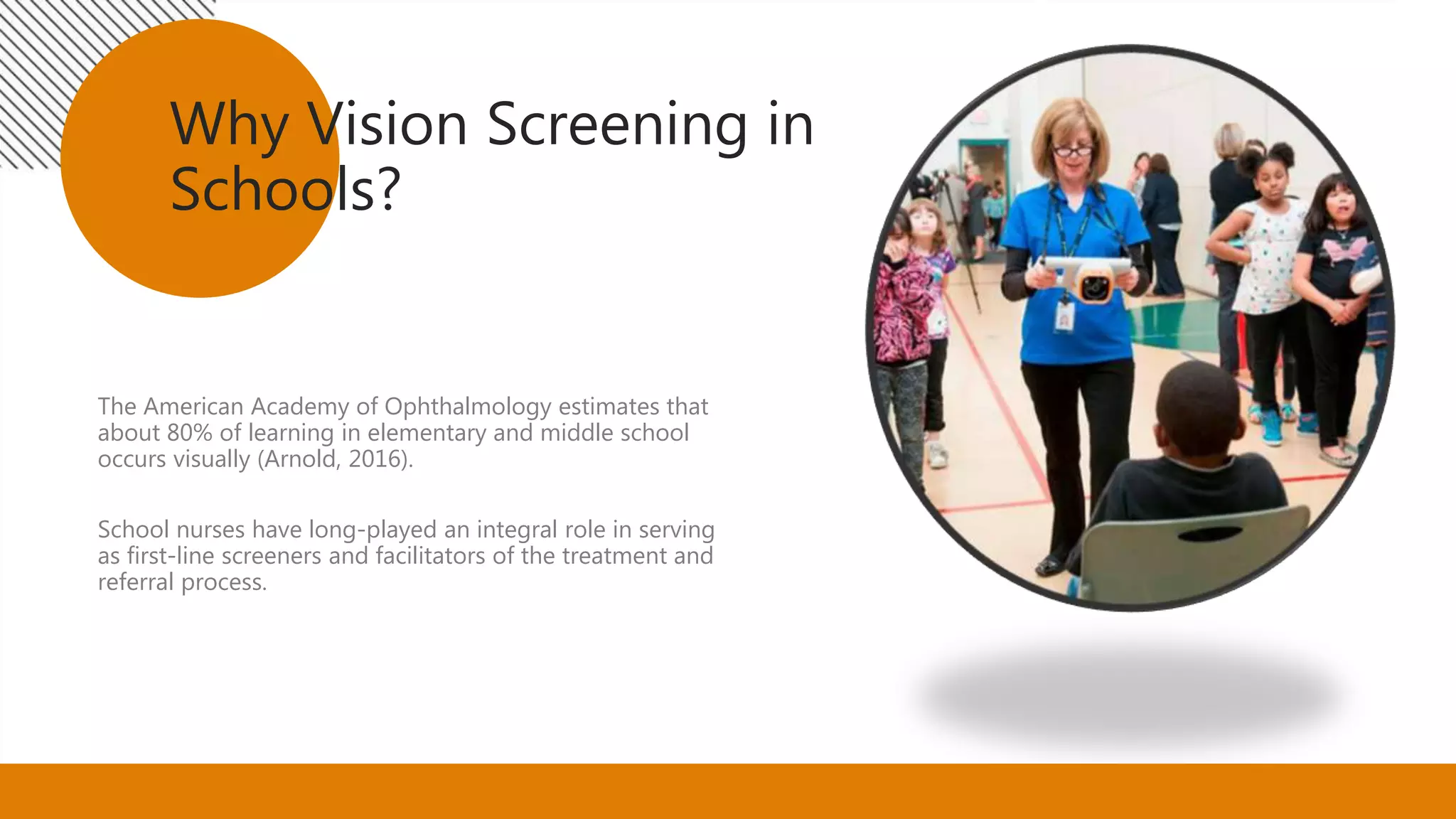
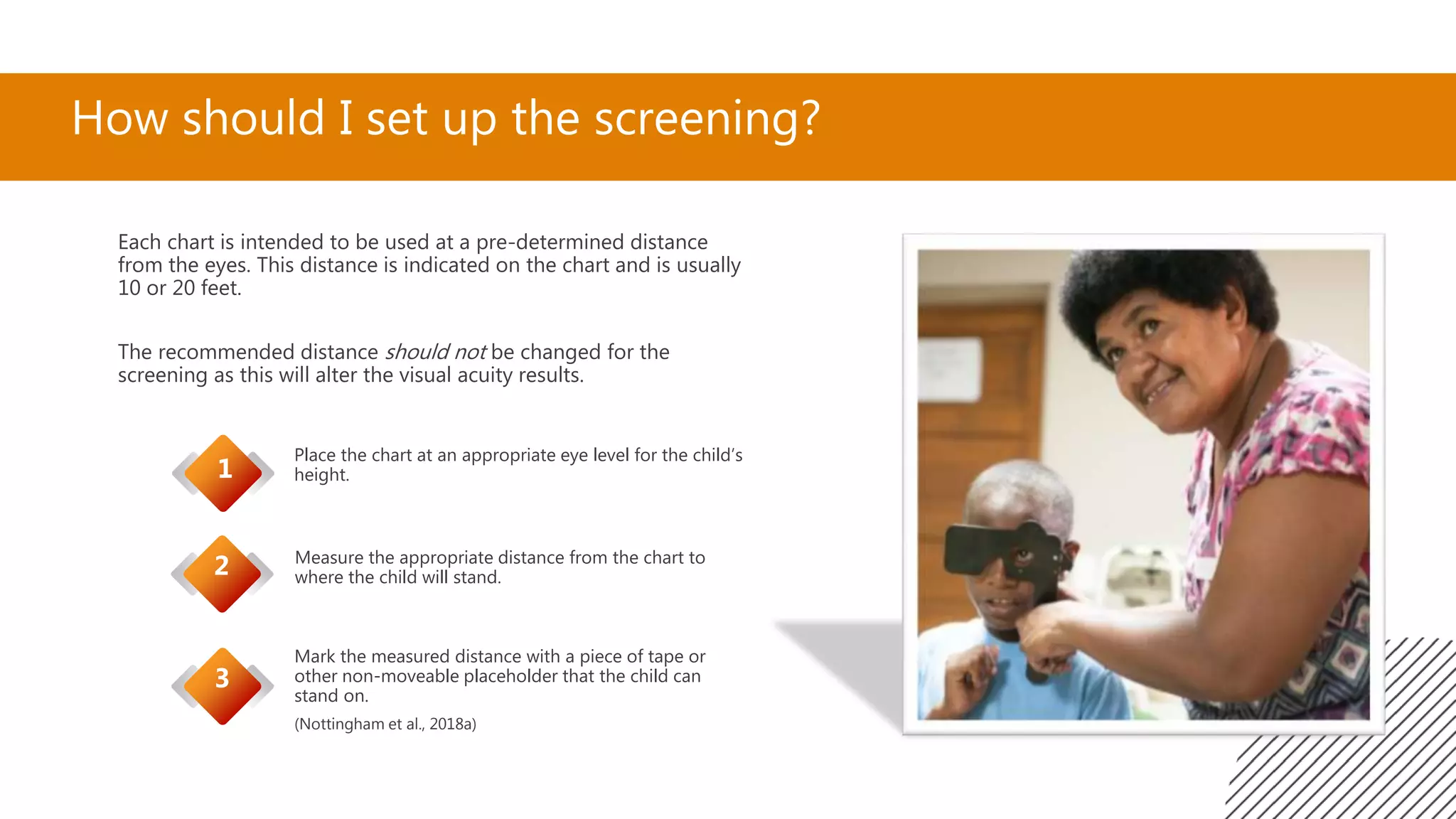
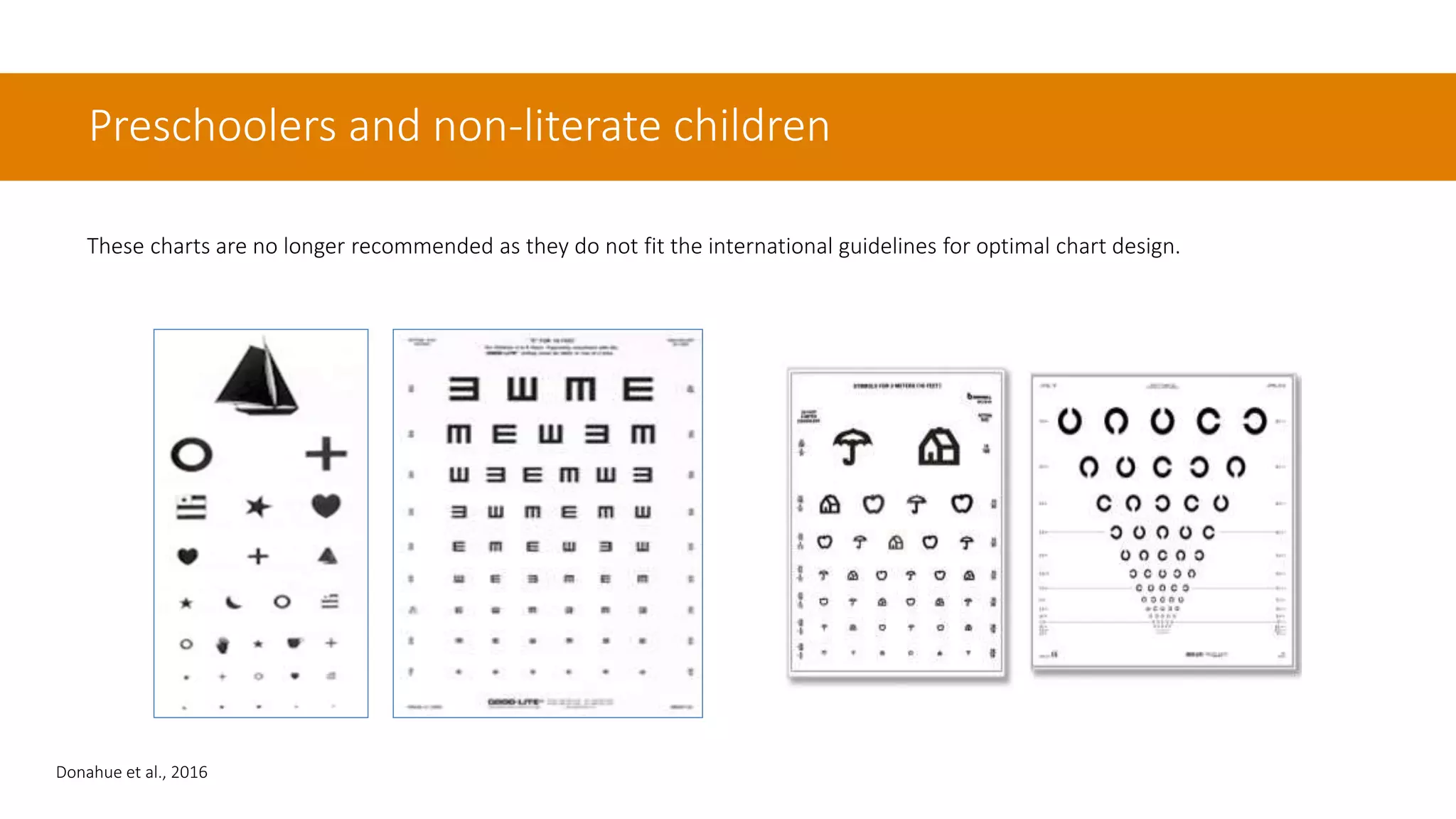
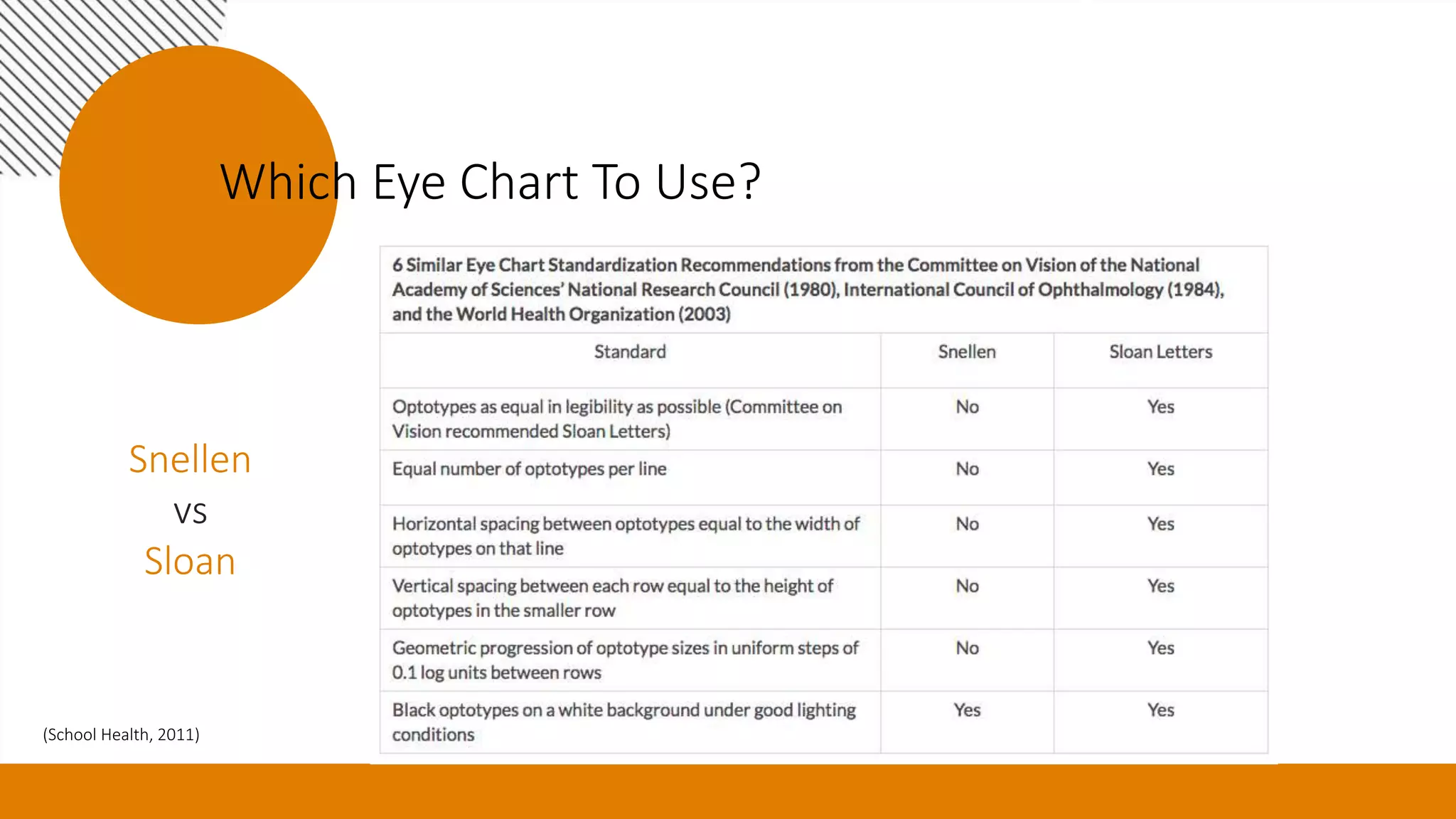
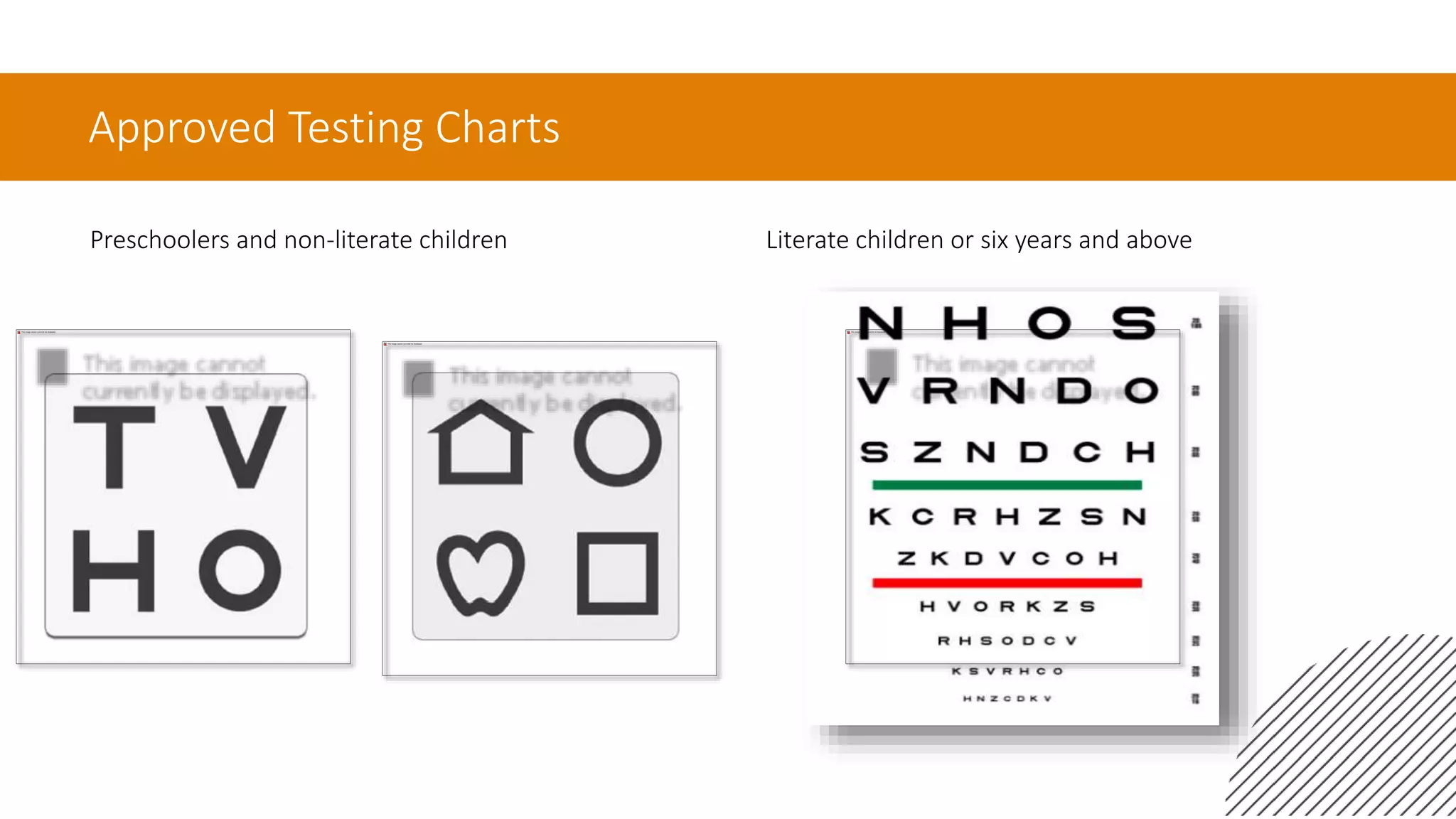
This document outlines updated guidelines for school-based vision screening, aimed at improving the detection of vision deficits in children. It emphasizes the role of school nurses in conducting visual acuity screenings and provides best practices including appropriate eye charts, occlusion techniques, and screening methods. Additionally, it discusses the importance of these screenings in relation to learning, as visual acuity significantly impacts educational outcomes.