- Basic newborn care (ENC) includes immediate care at birth, care during the first day and up to 28 days to support survival and wellbeing.
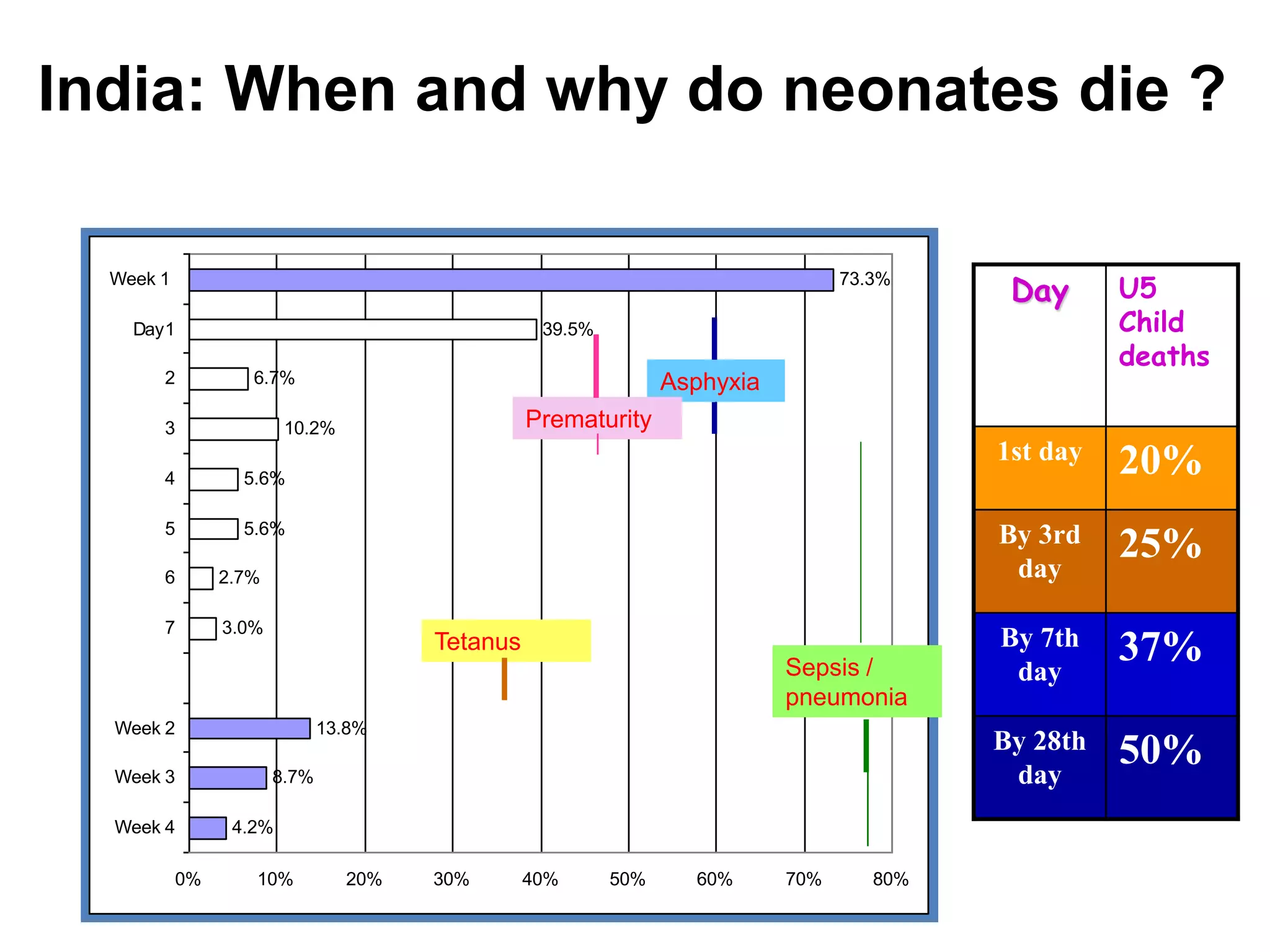
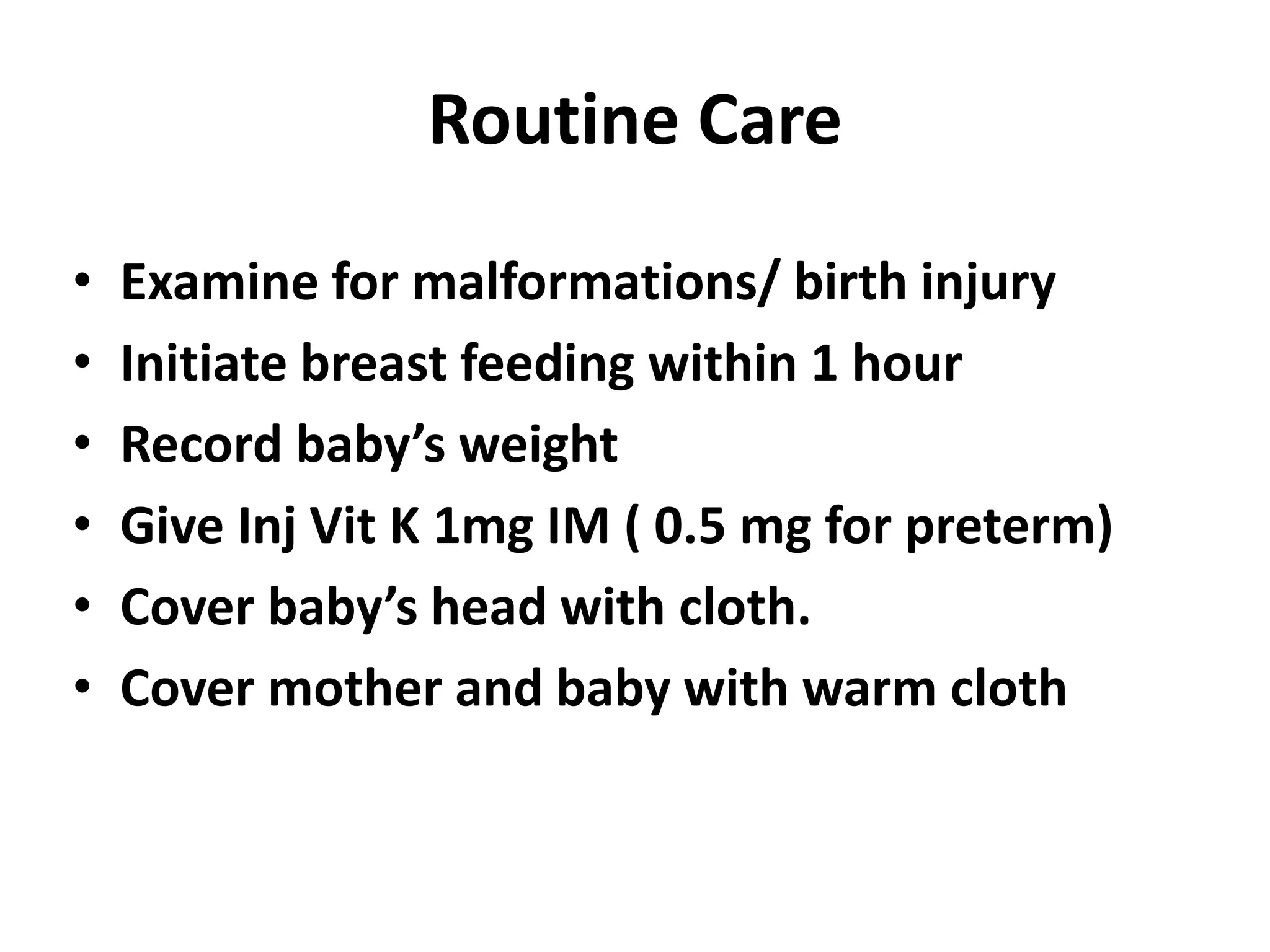
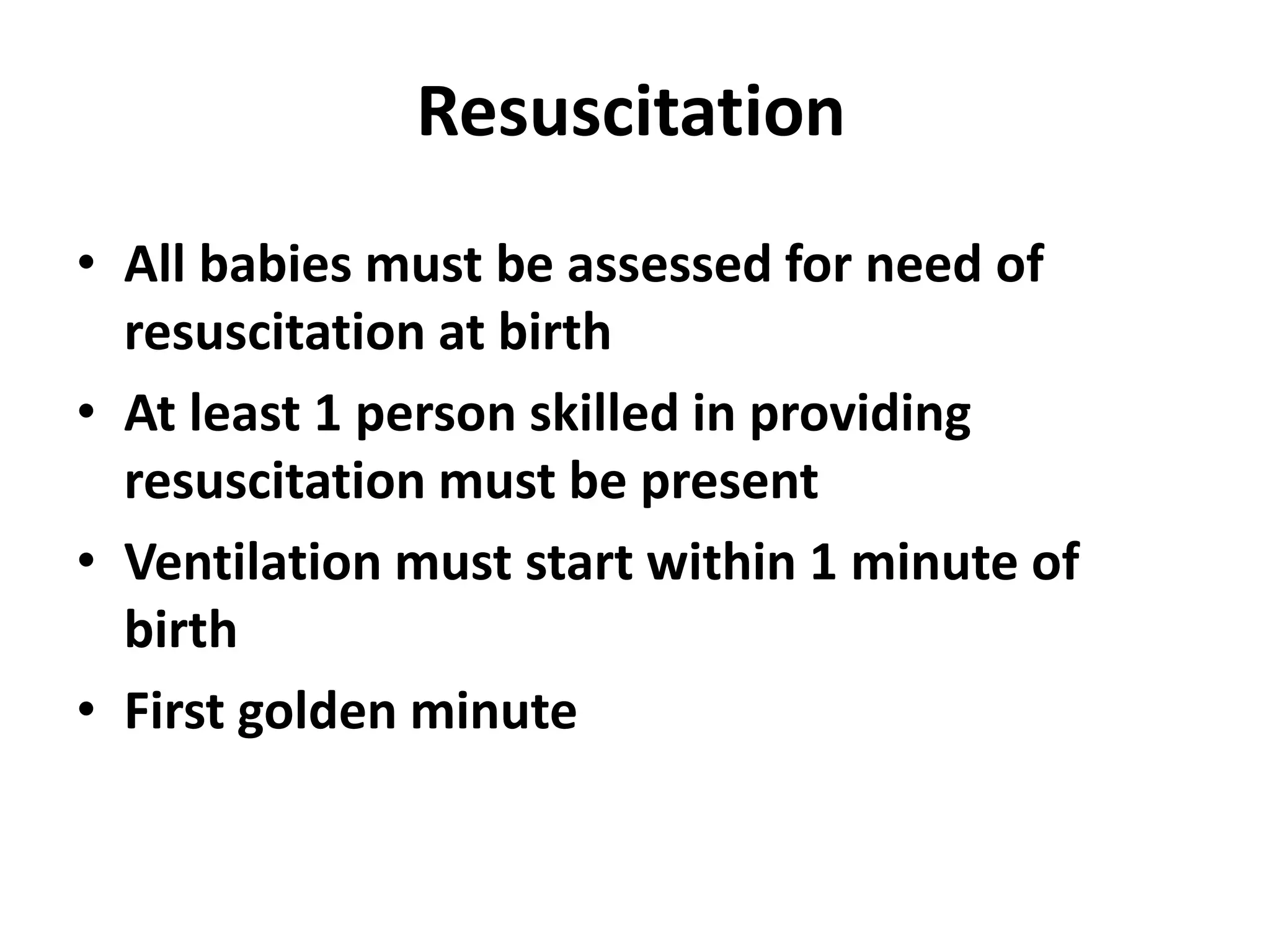
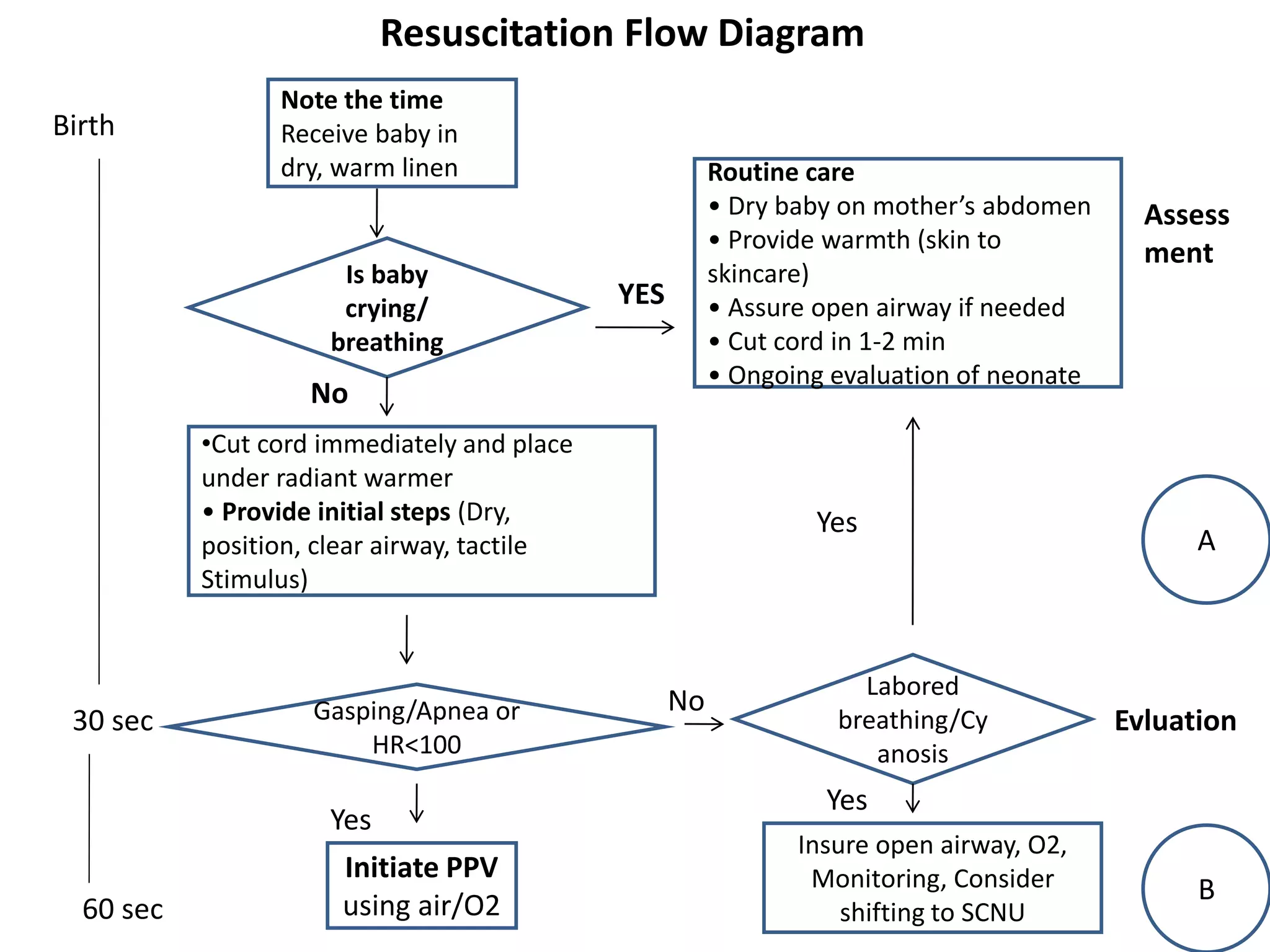
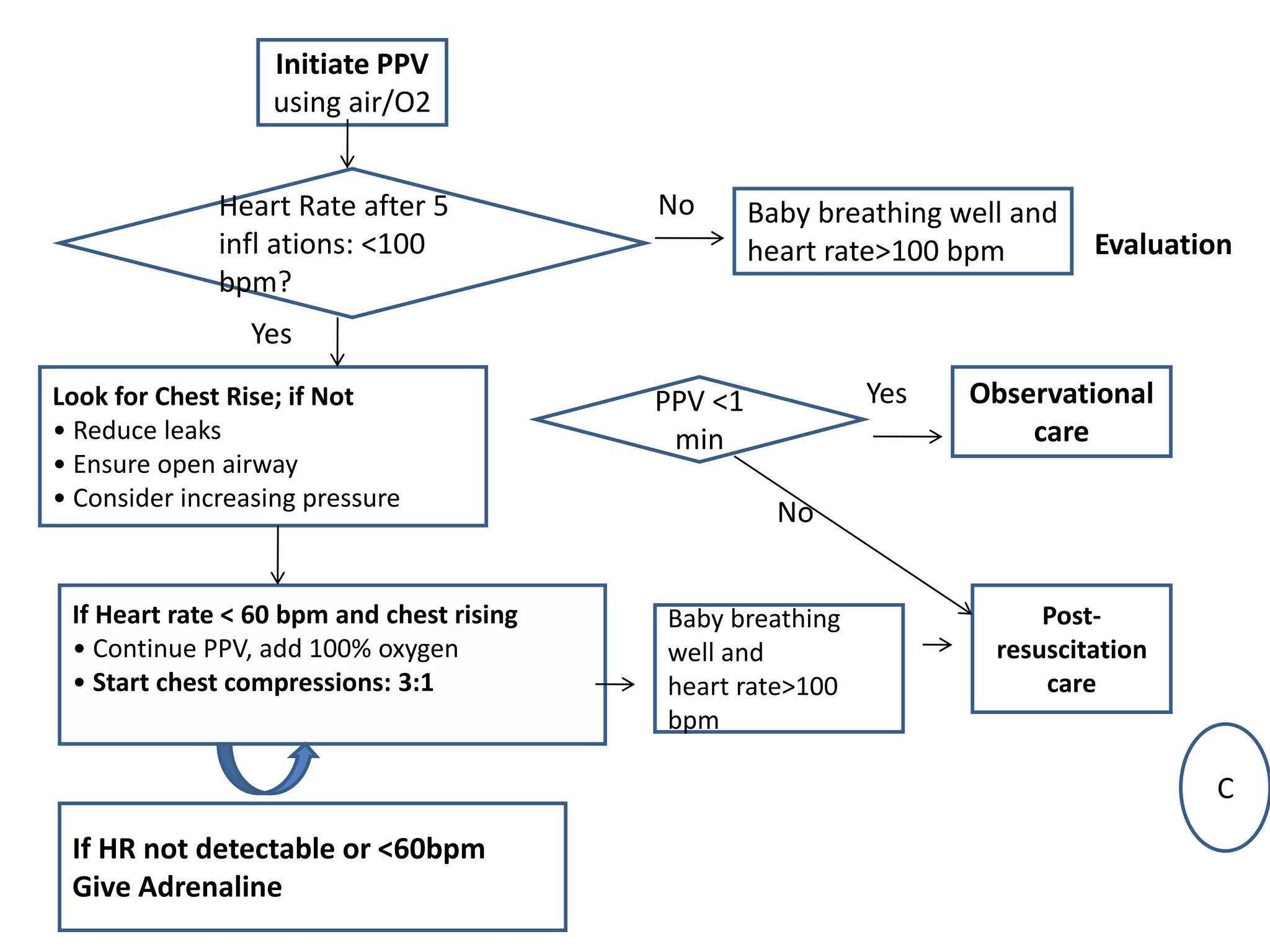
- Ventilation must be initiated within 1 minute of birth, and all efforts should be made to help the mother initiate breastfeeding within the first hour.
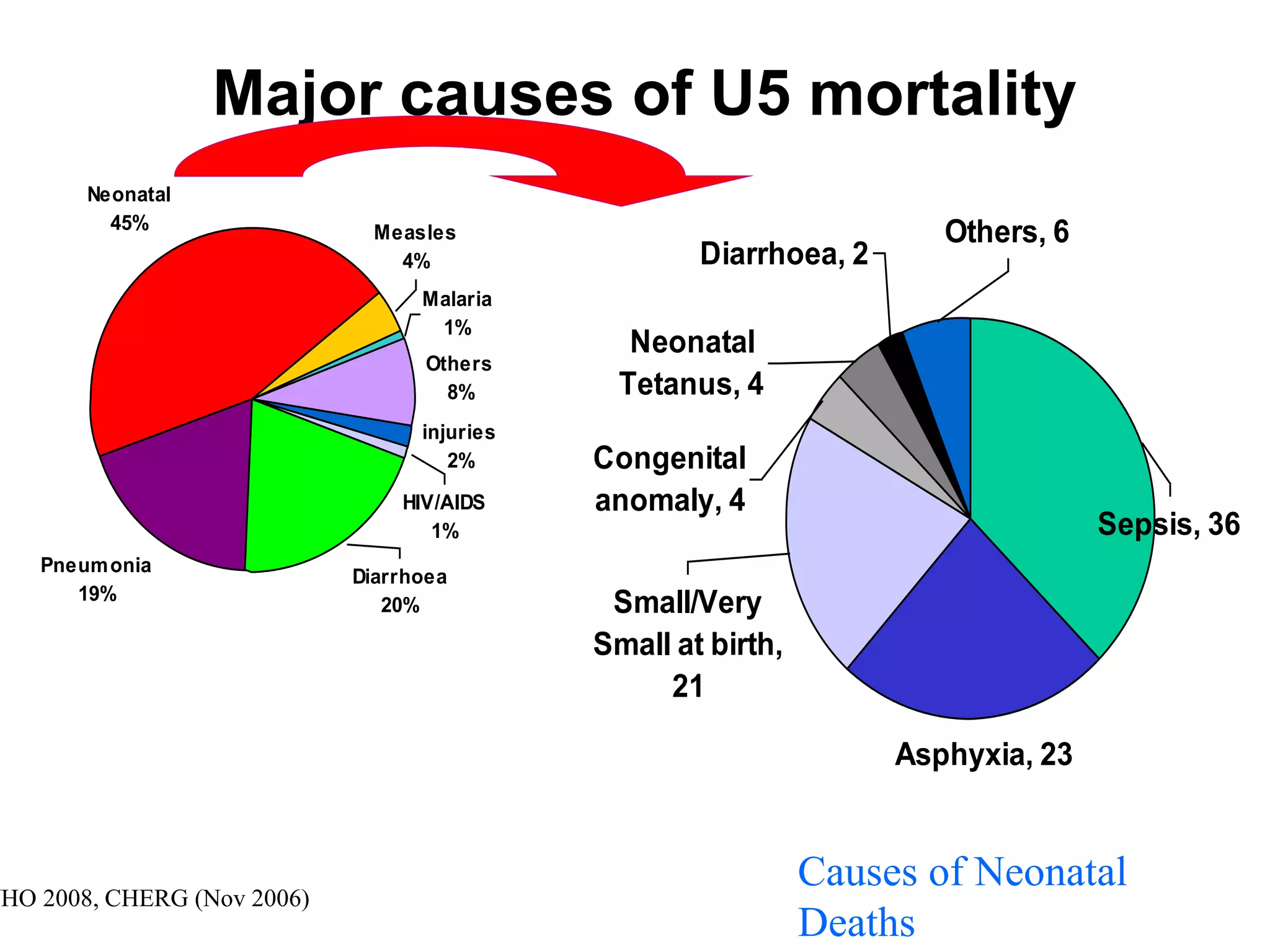
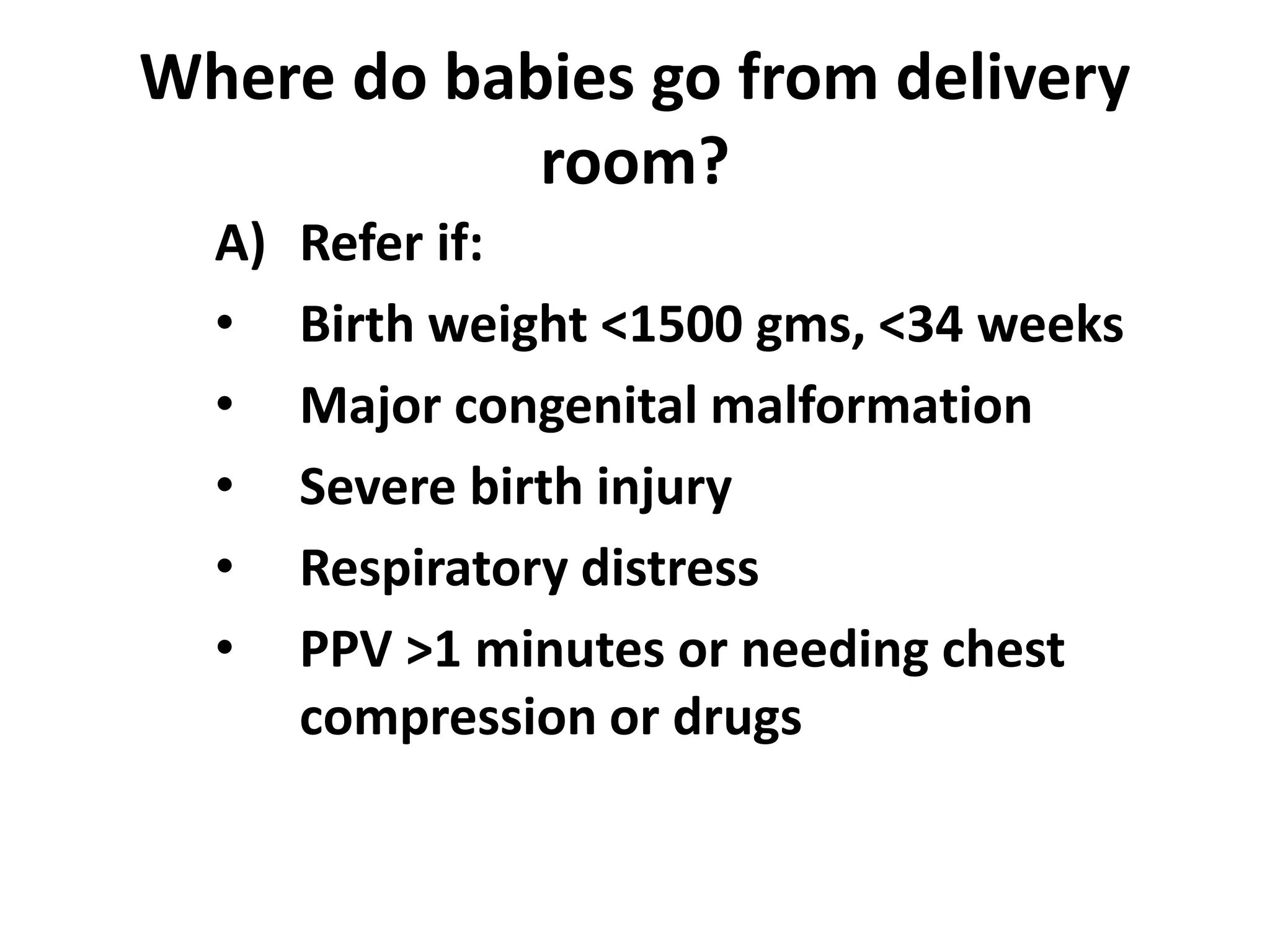
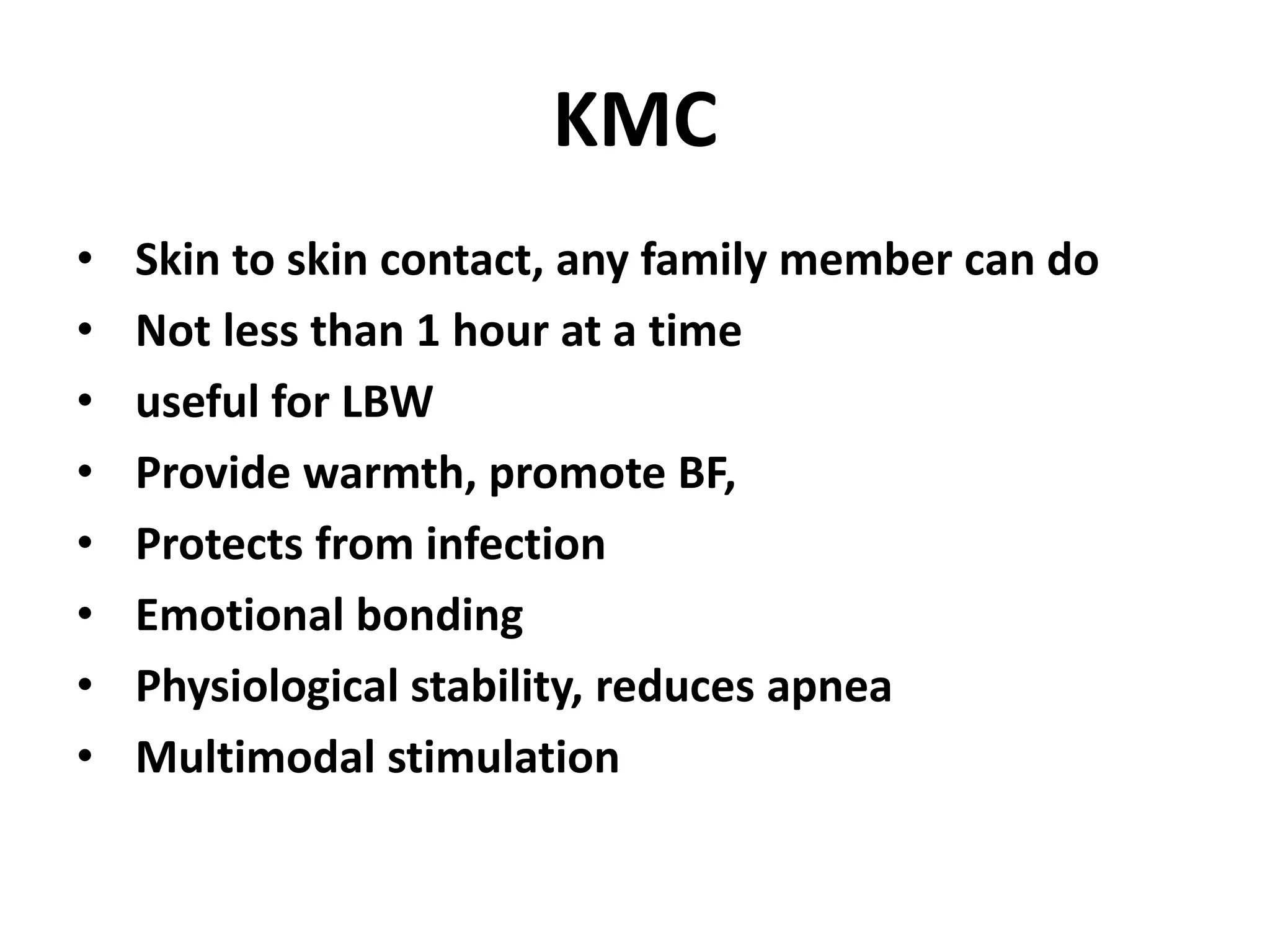
- Newborns requiring special care, such as those born prematurely or with low birth weight, should be identified and referred appropriately.
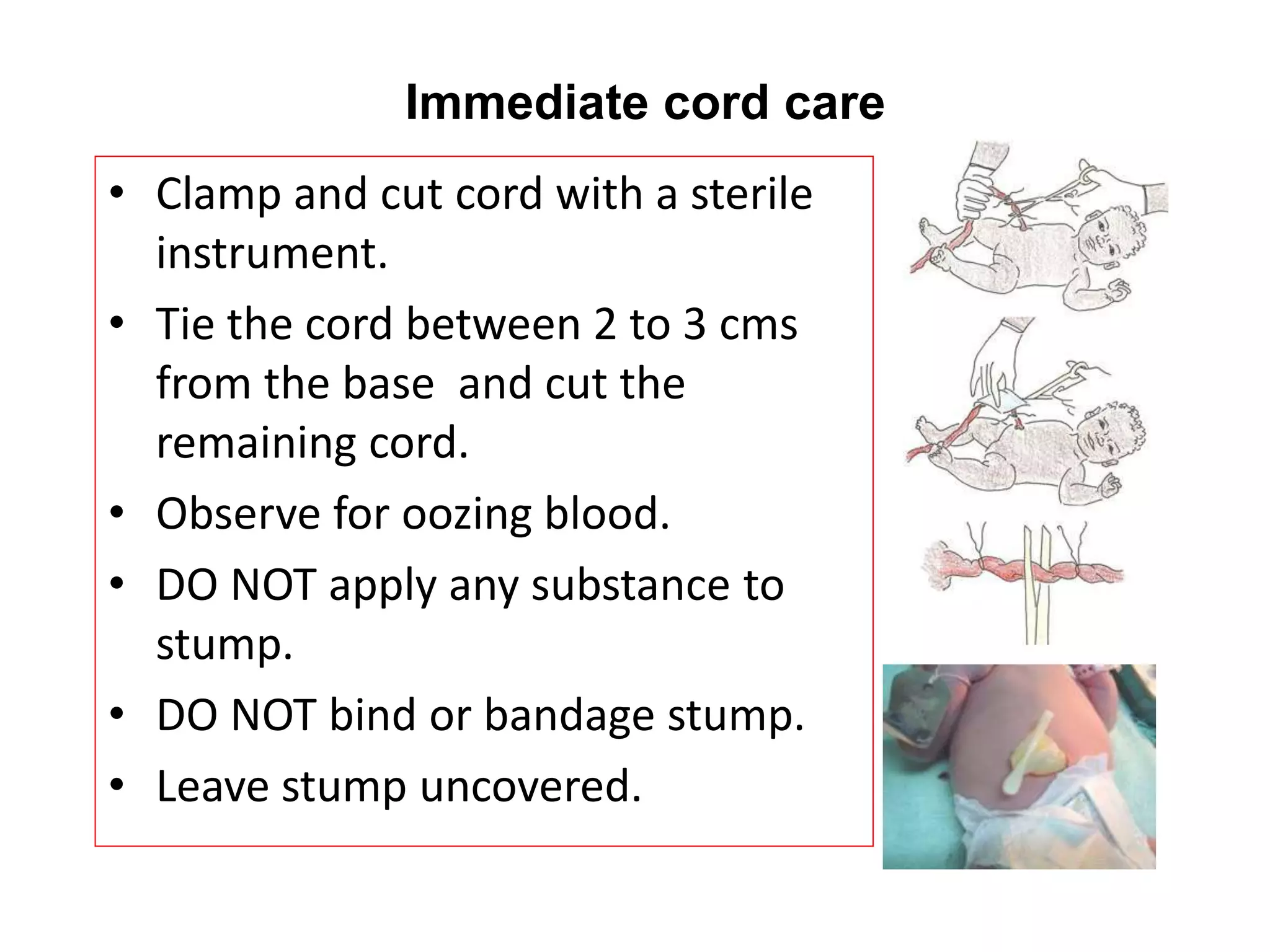
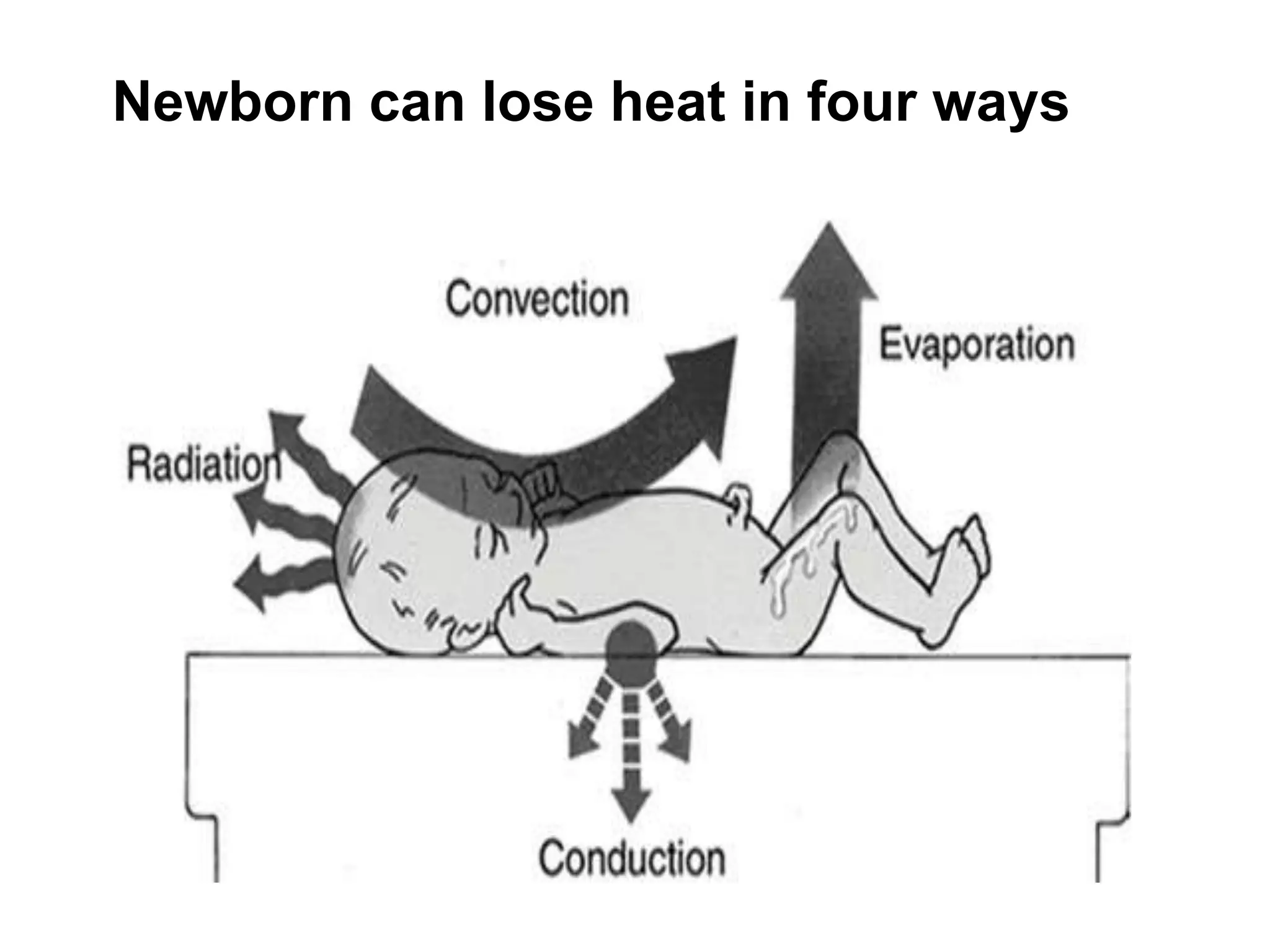
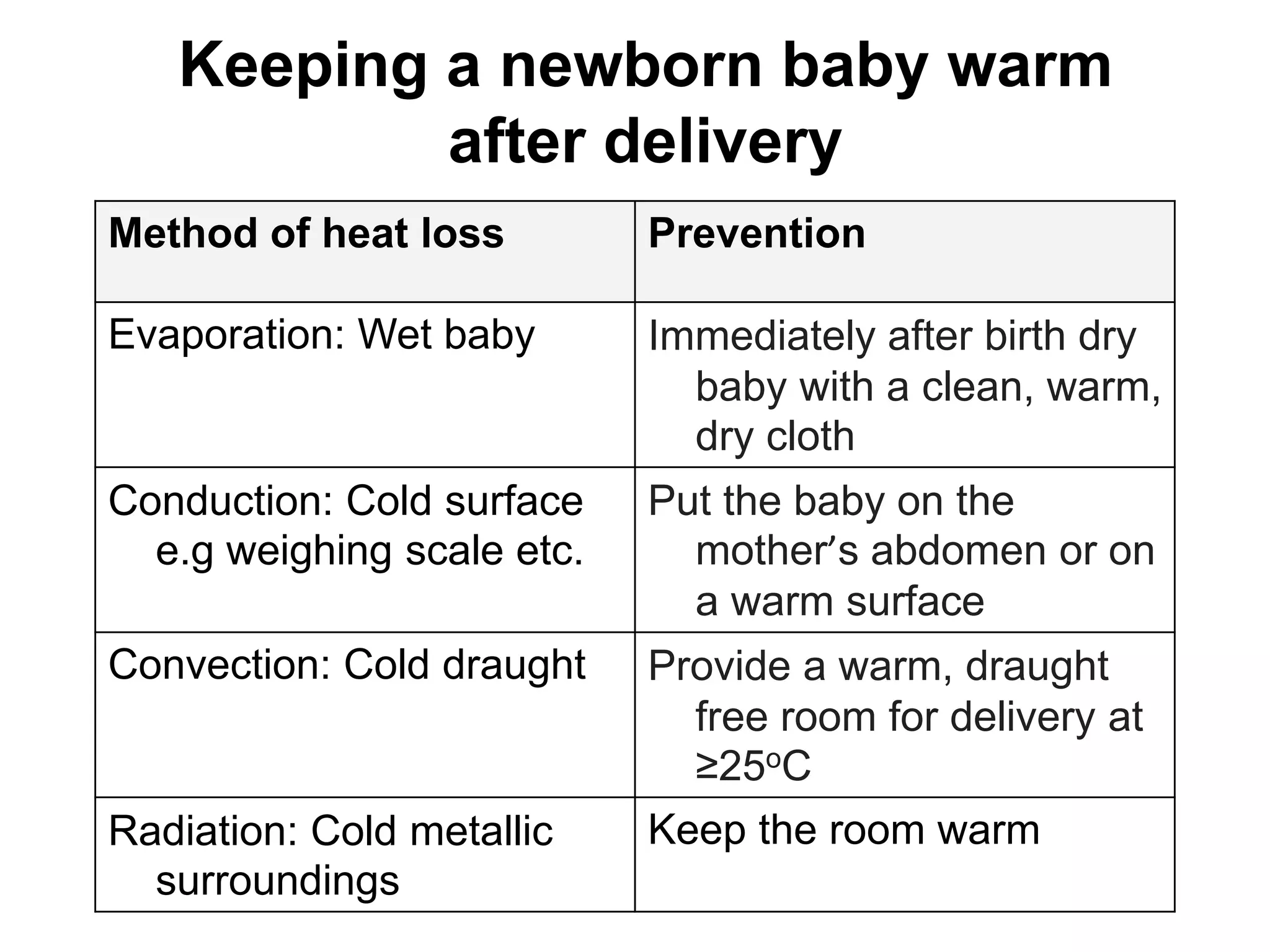
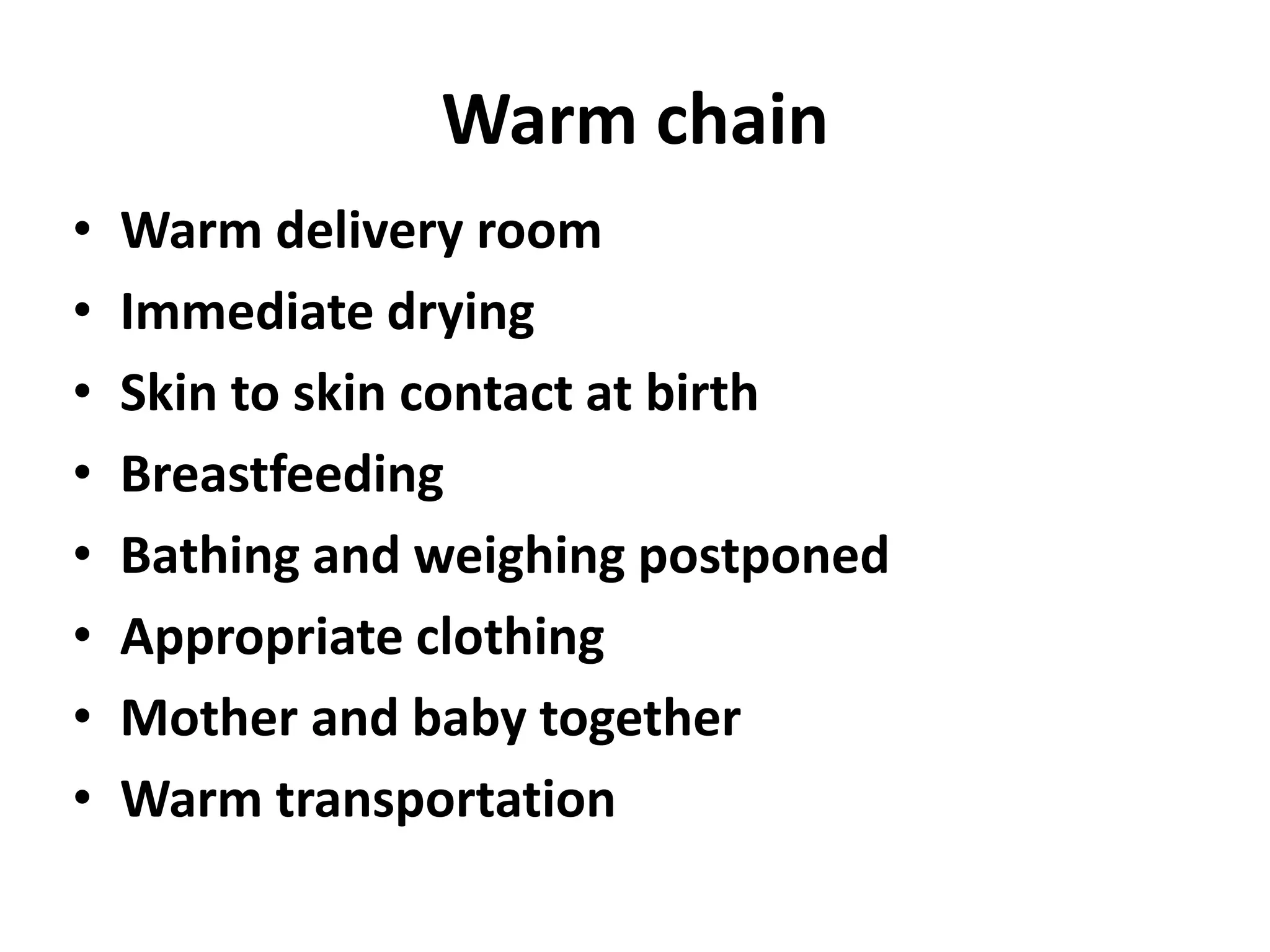
- All precautions must be taken to prevent infection, hypothermia, and the mother should be counseled on danger signs and the importance of follow-up visits and immunizations.