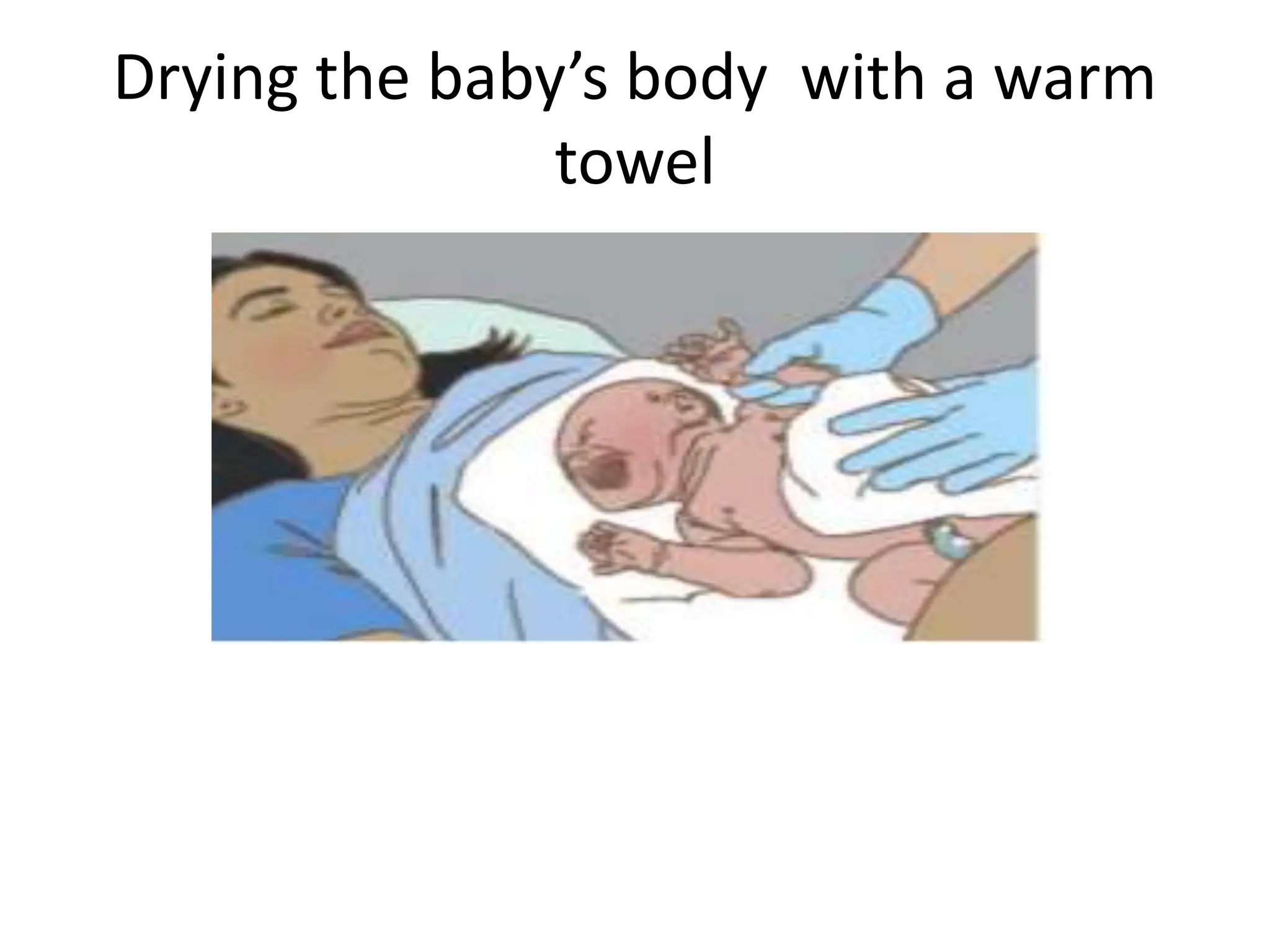
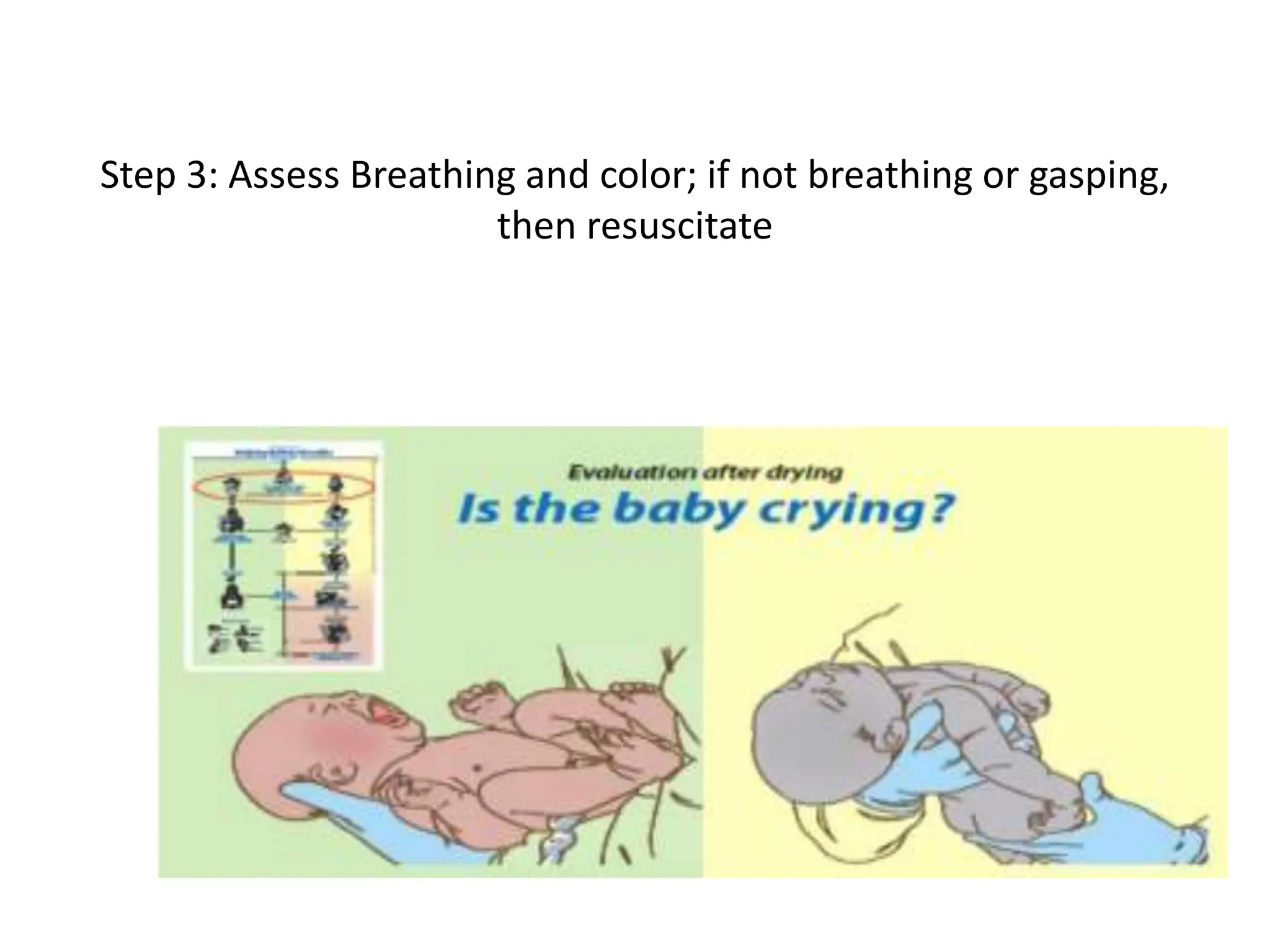
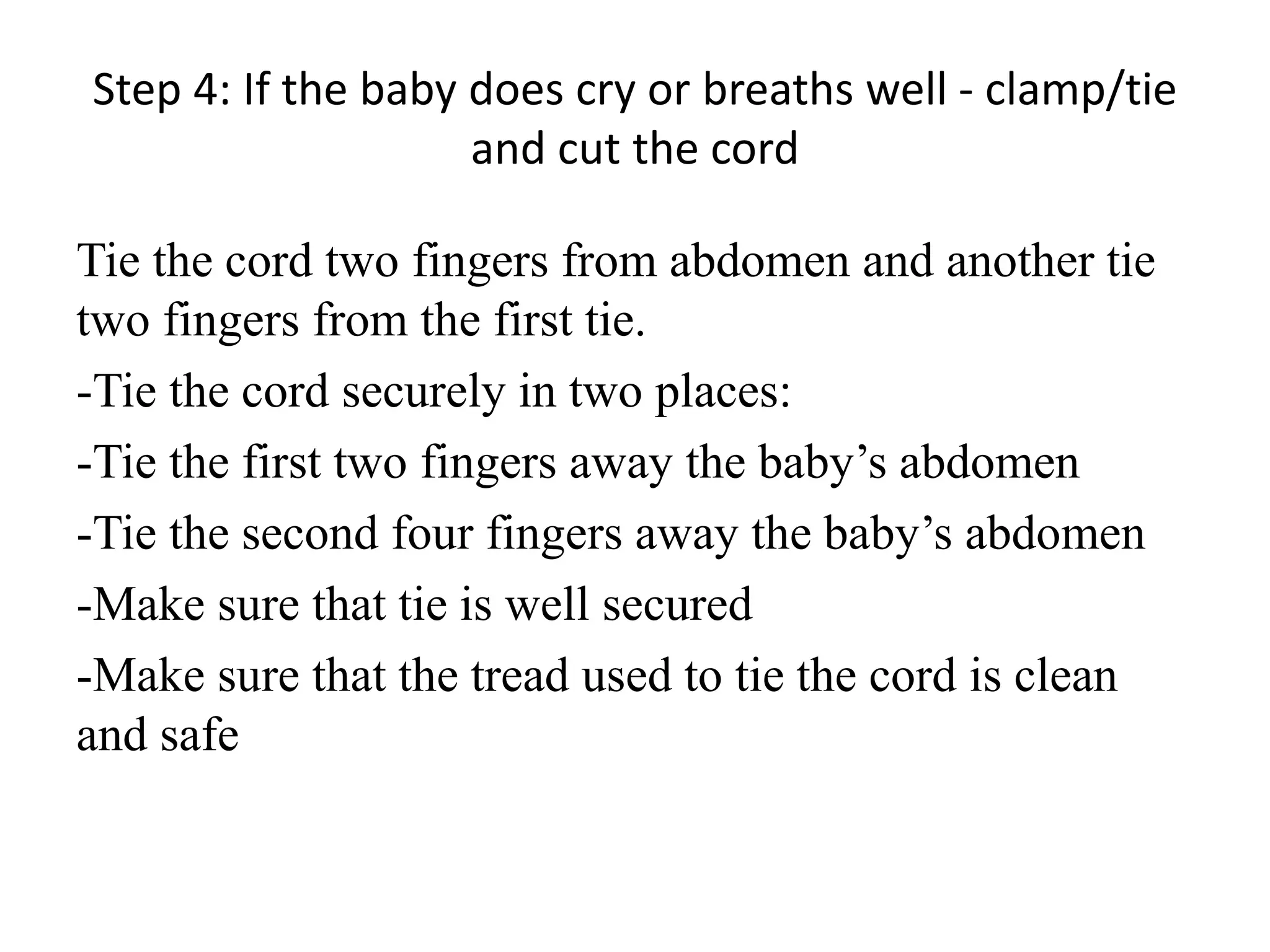
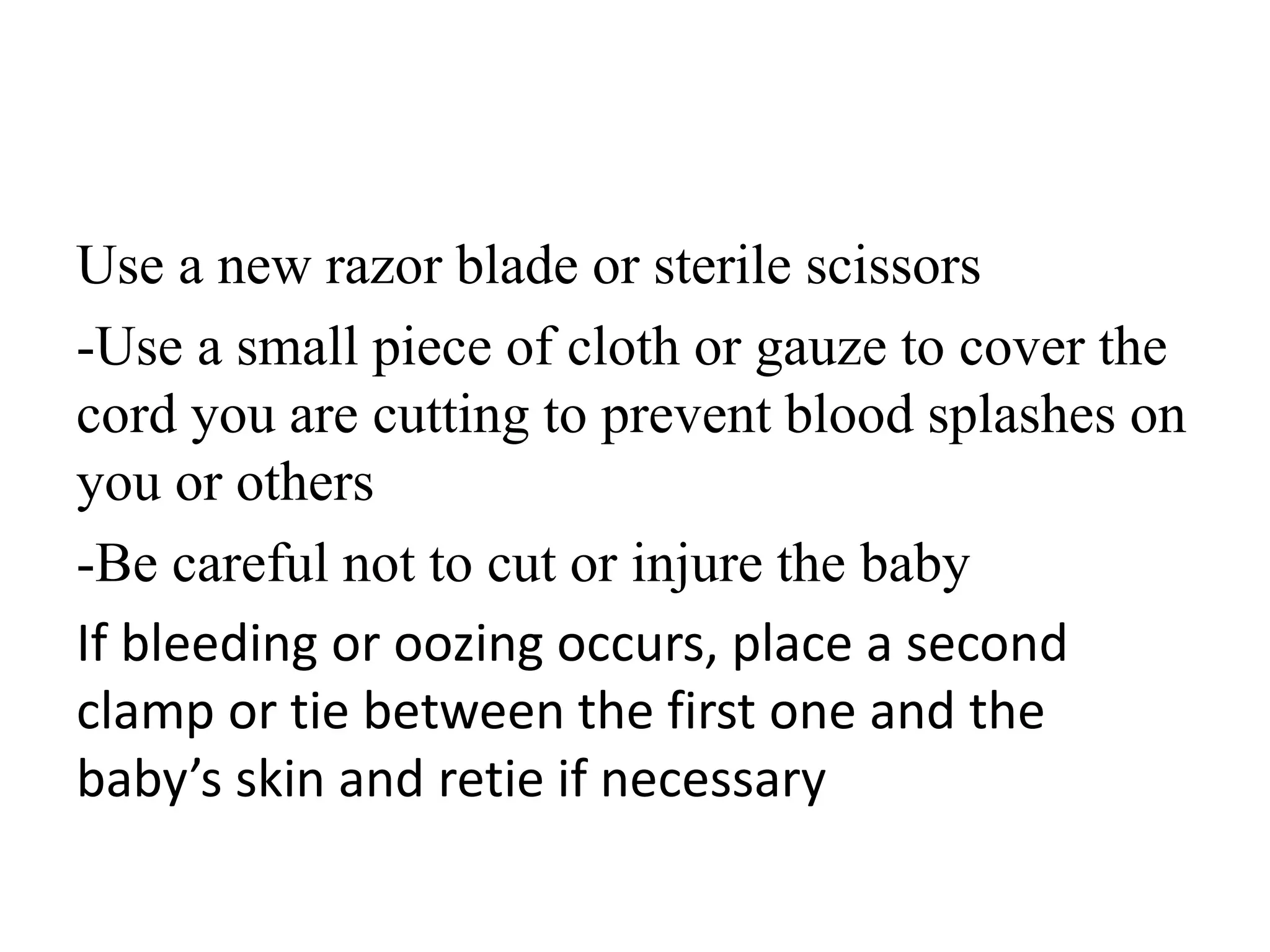
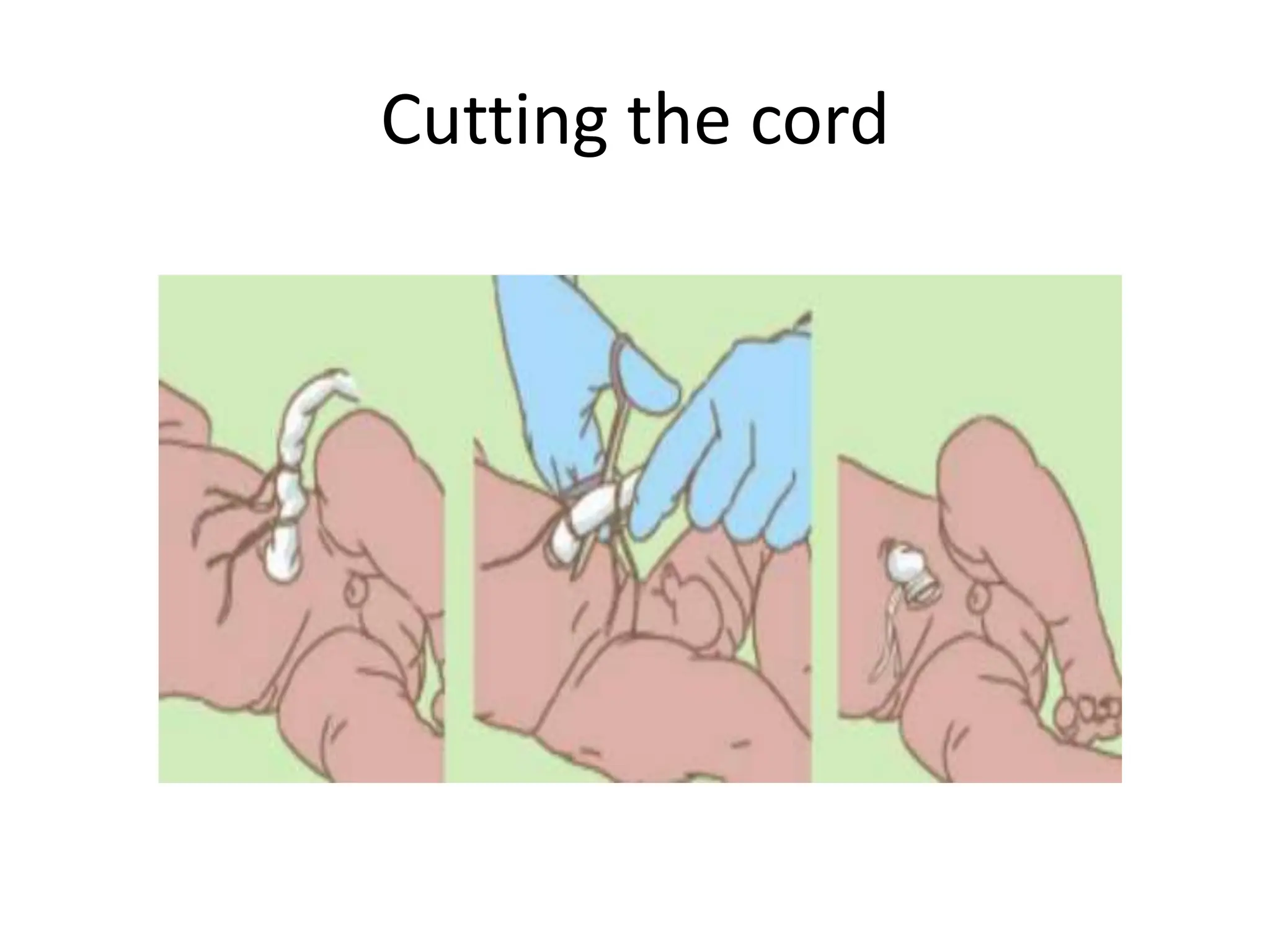
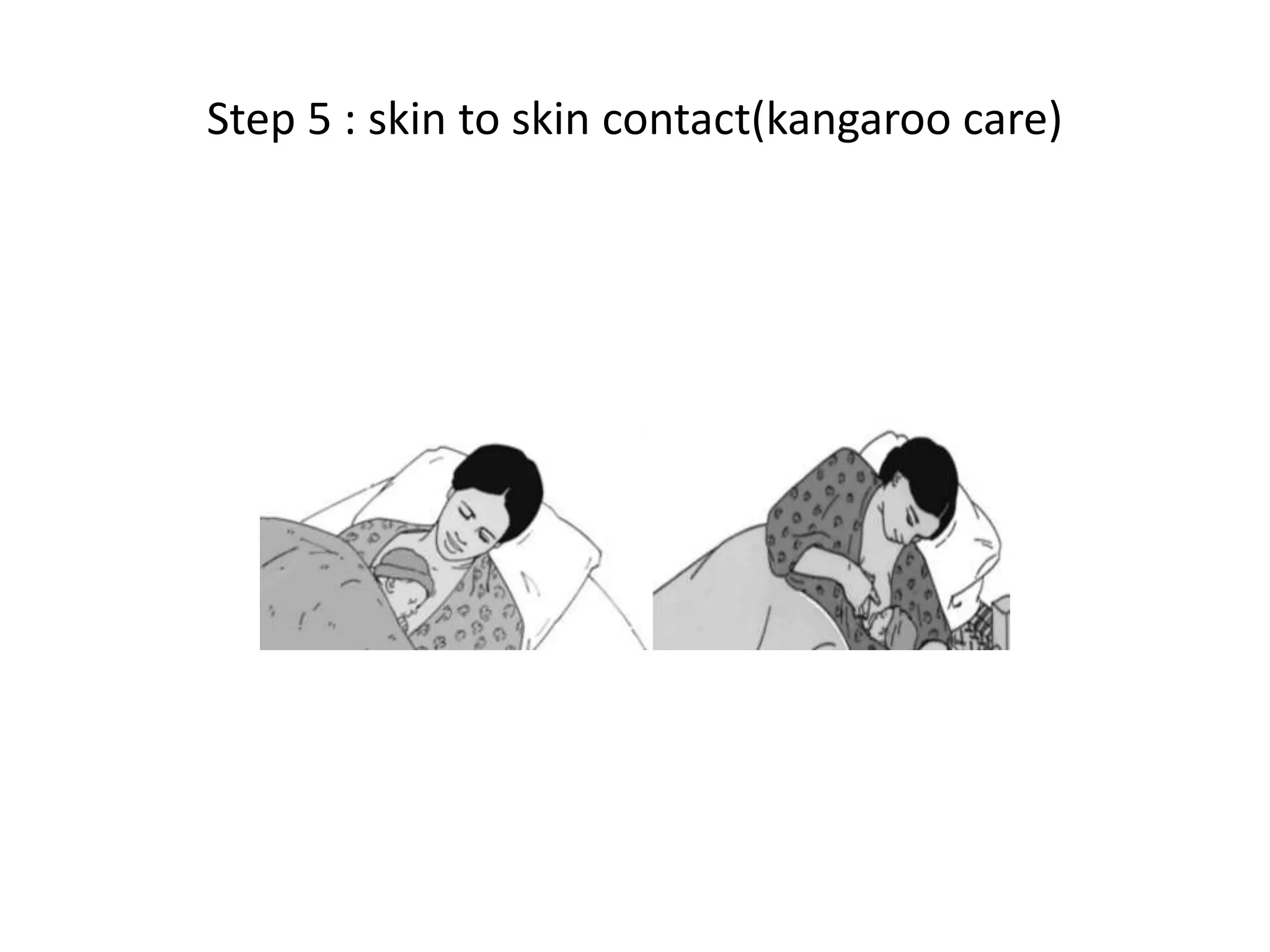
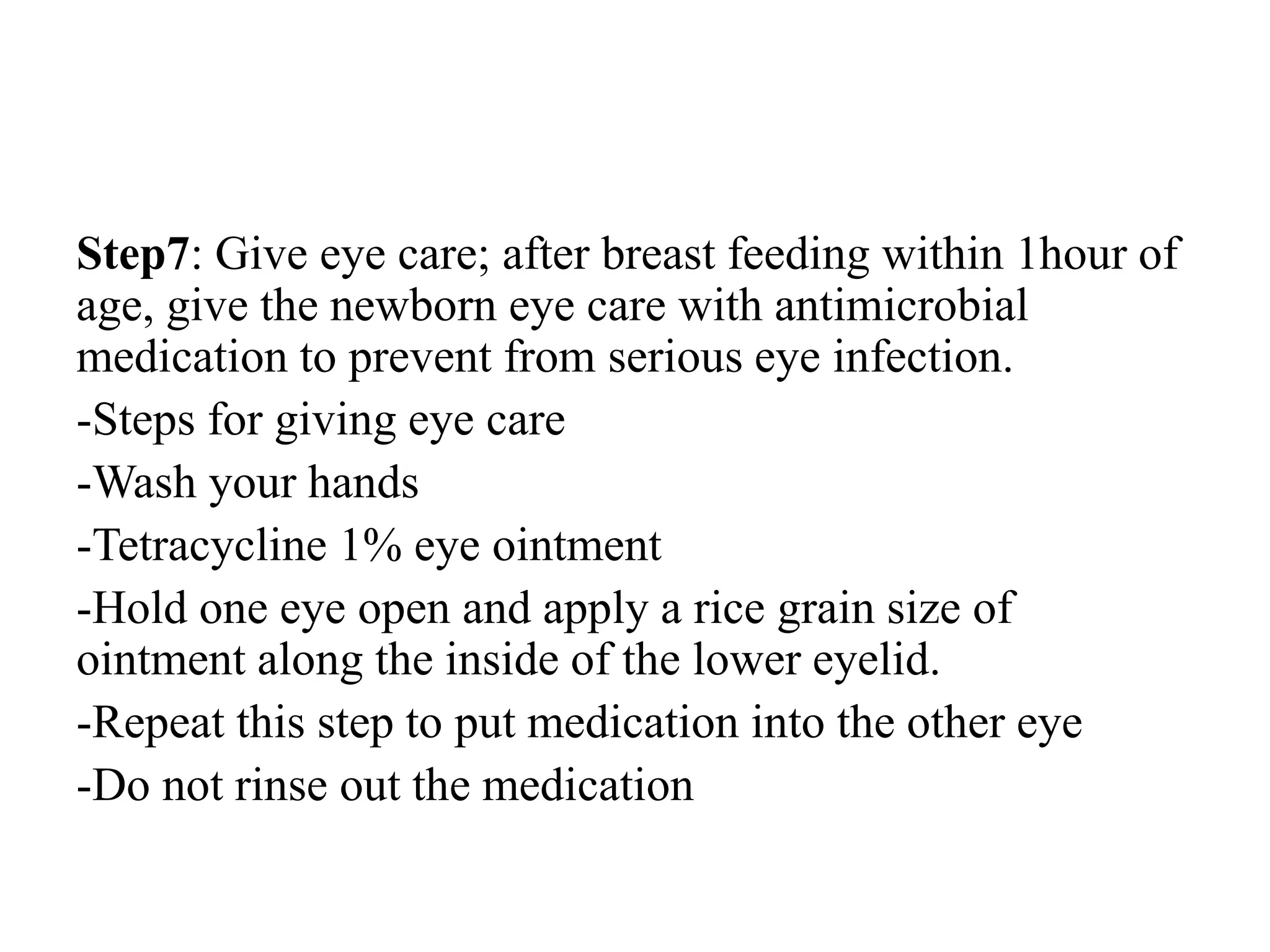
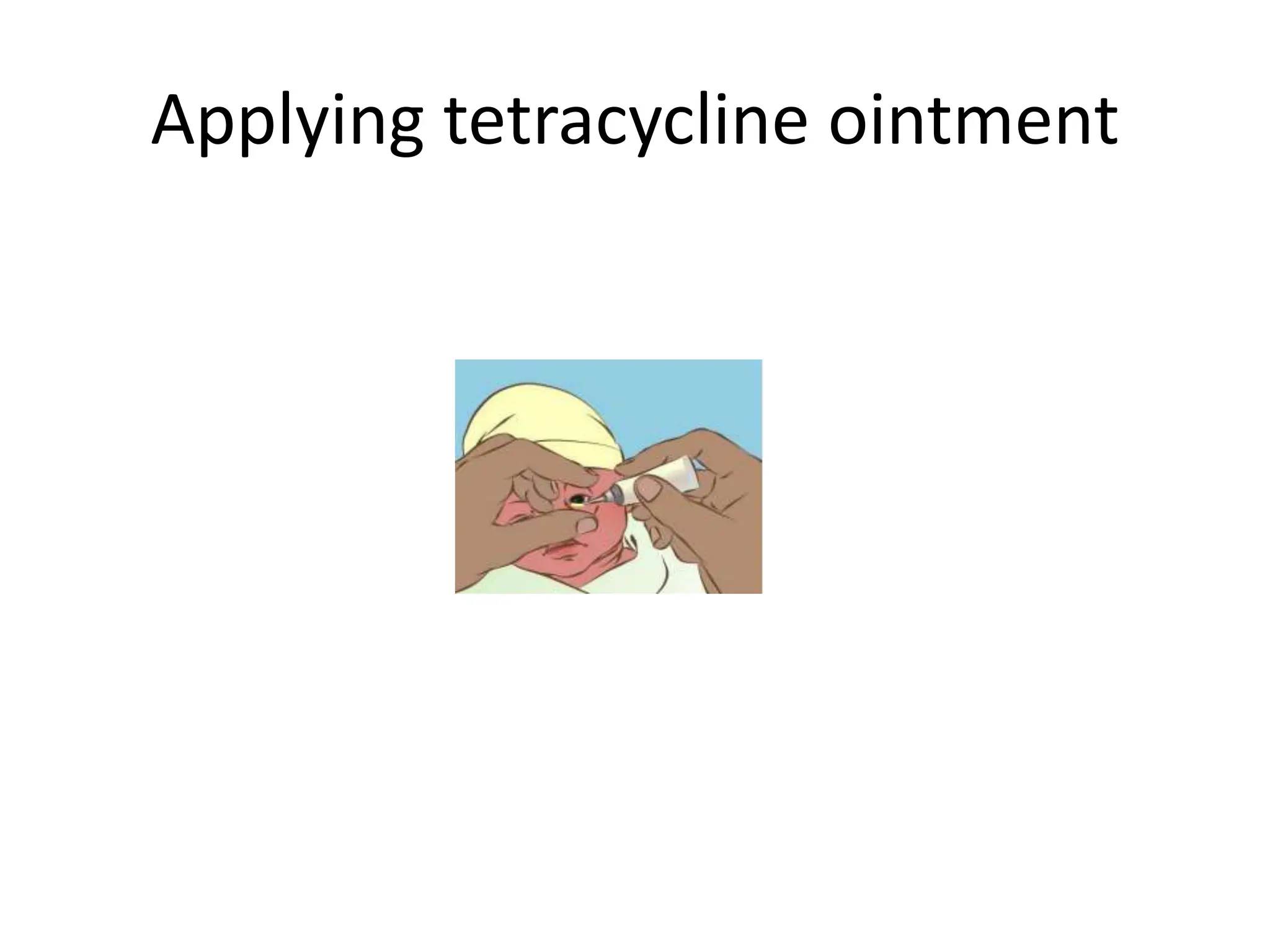
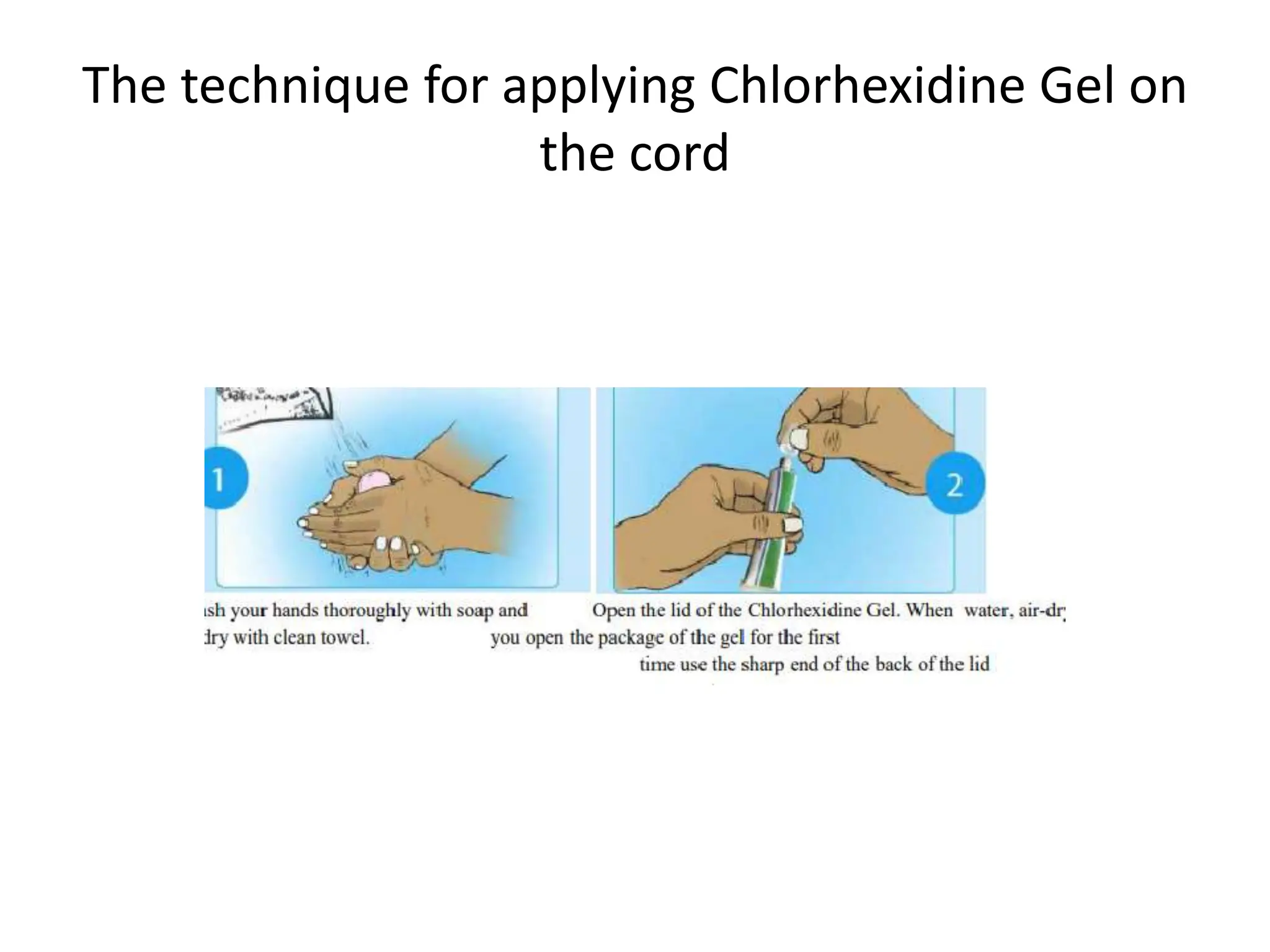
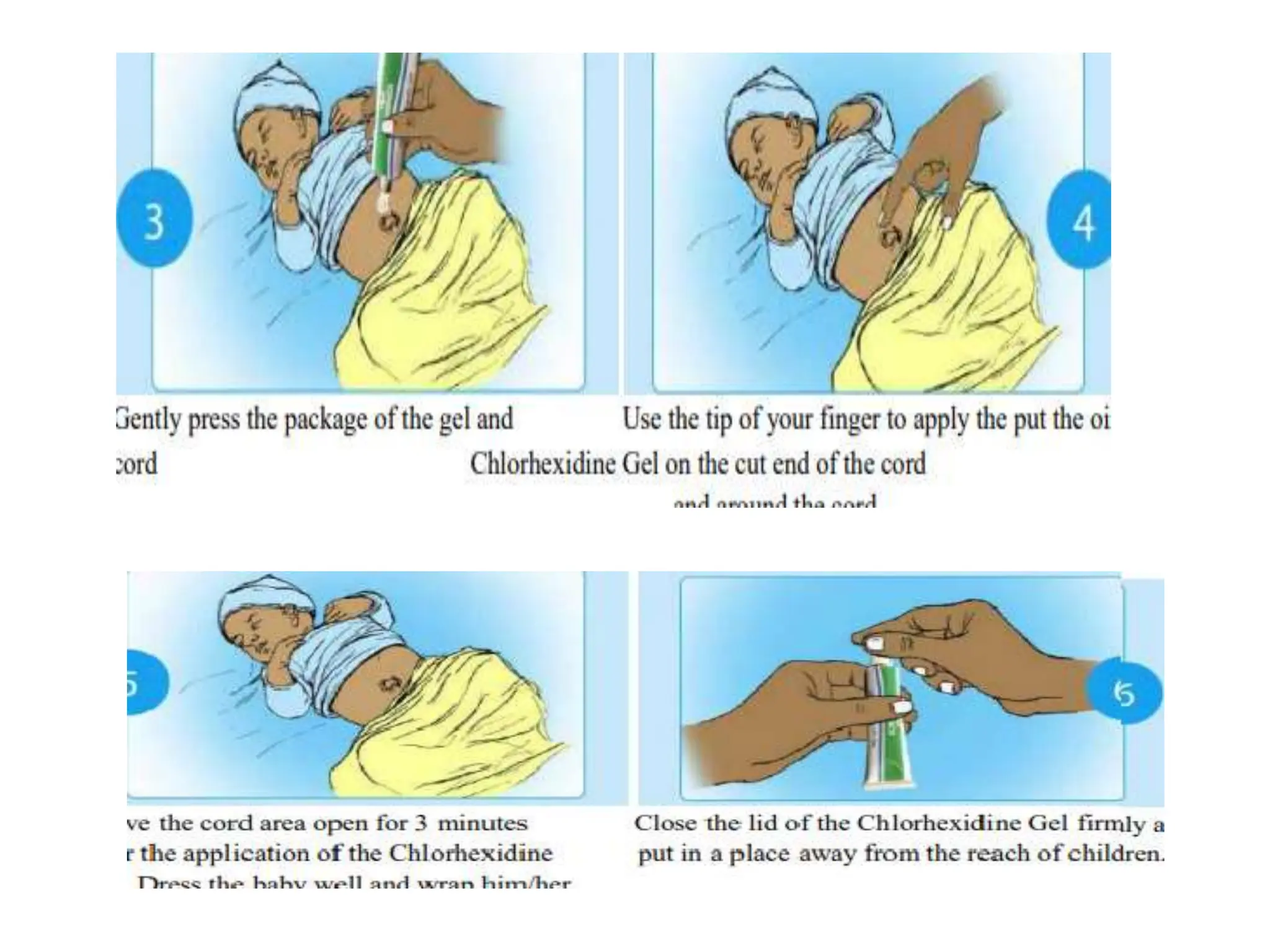
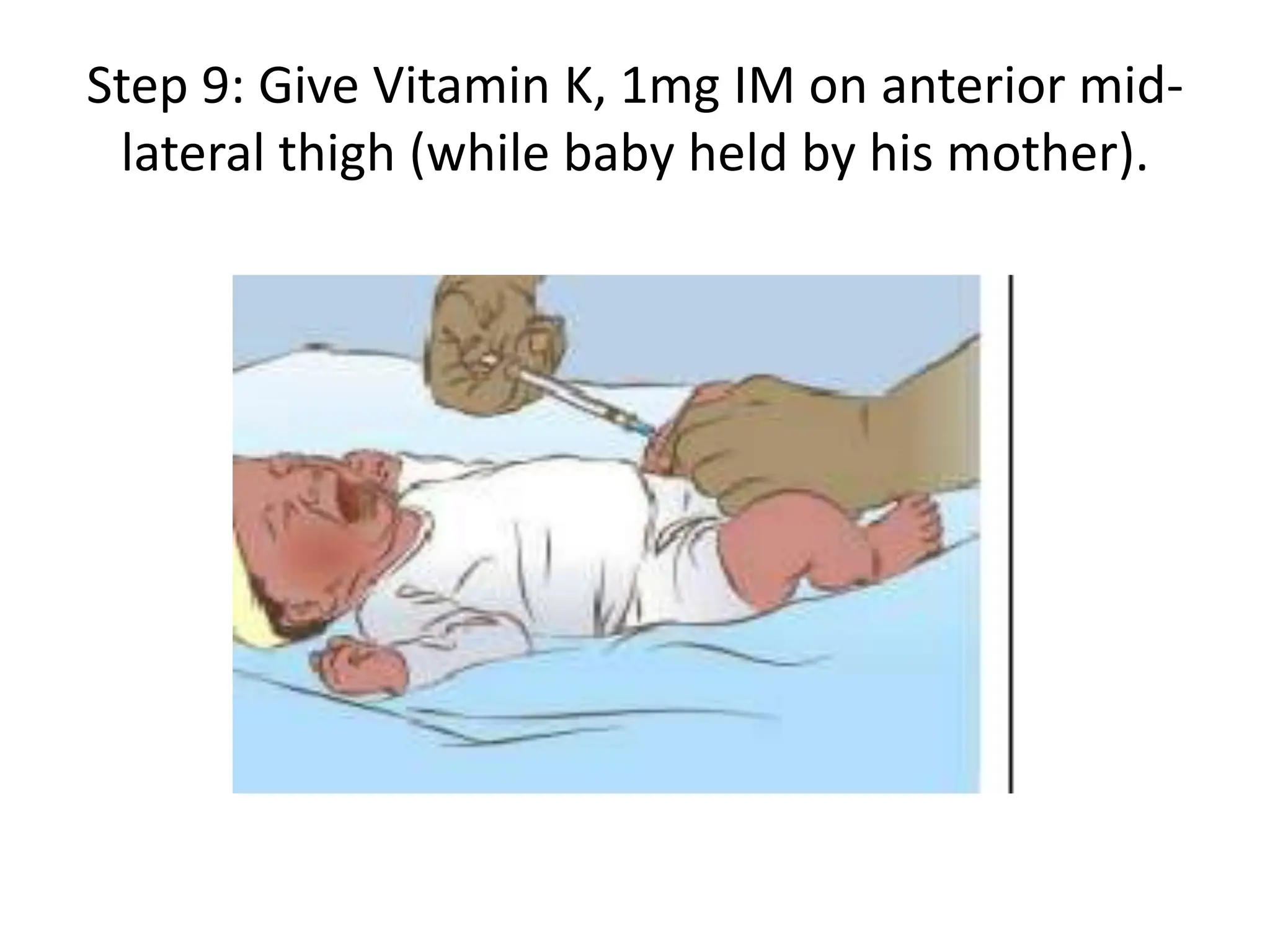
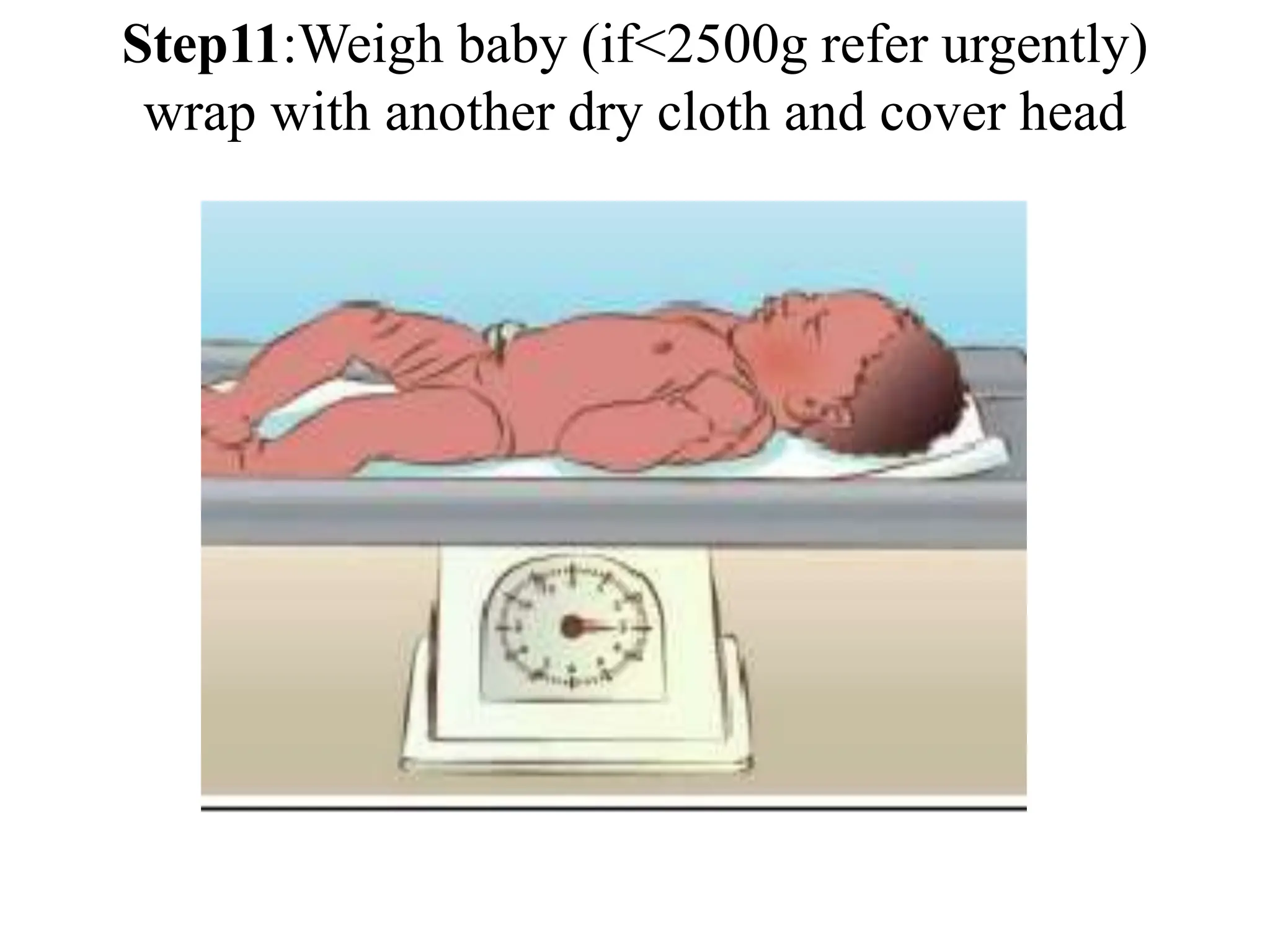
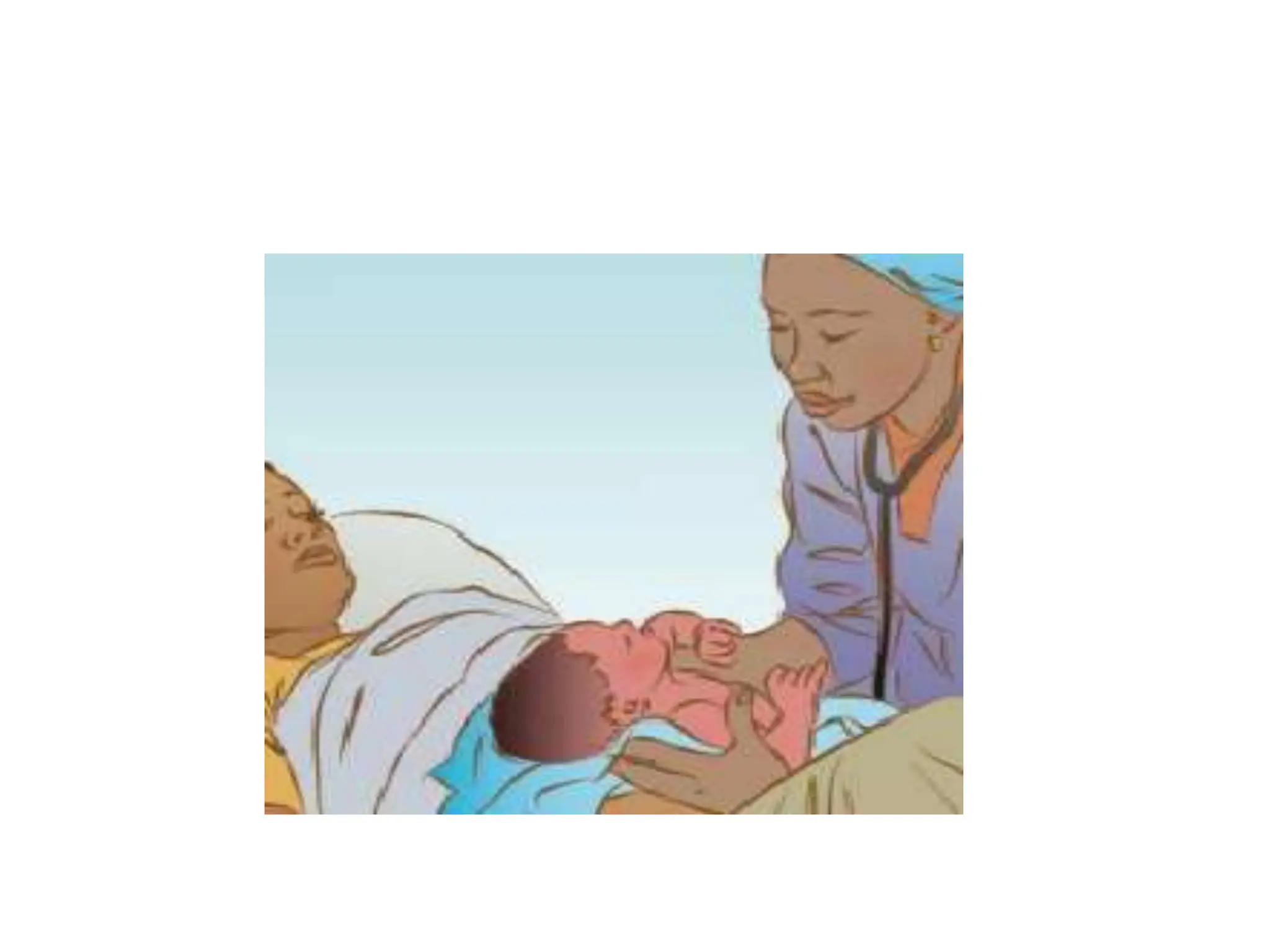
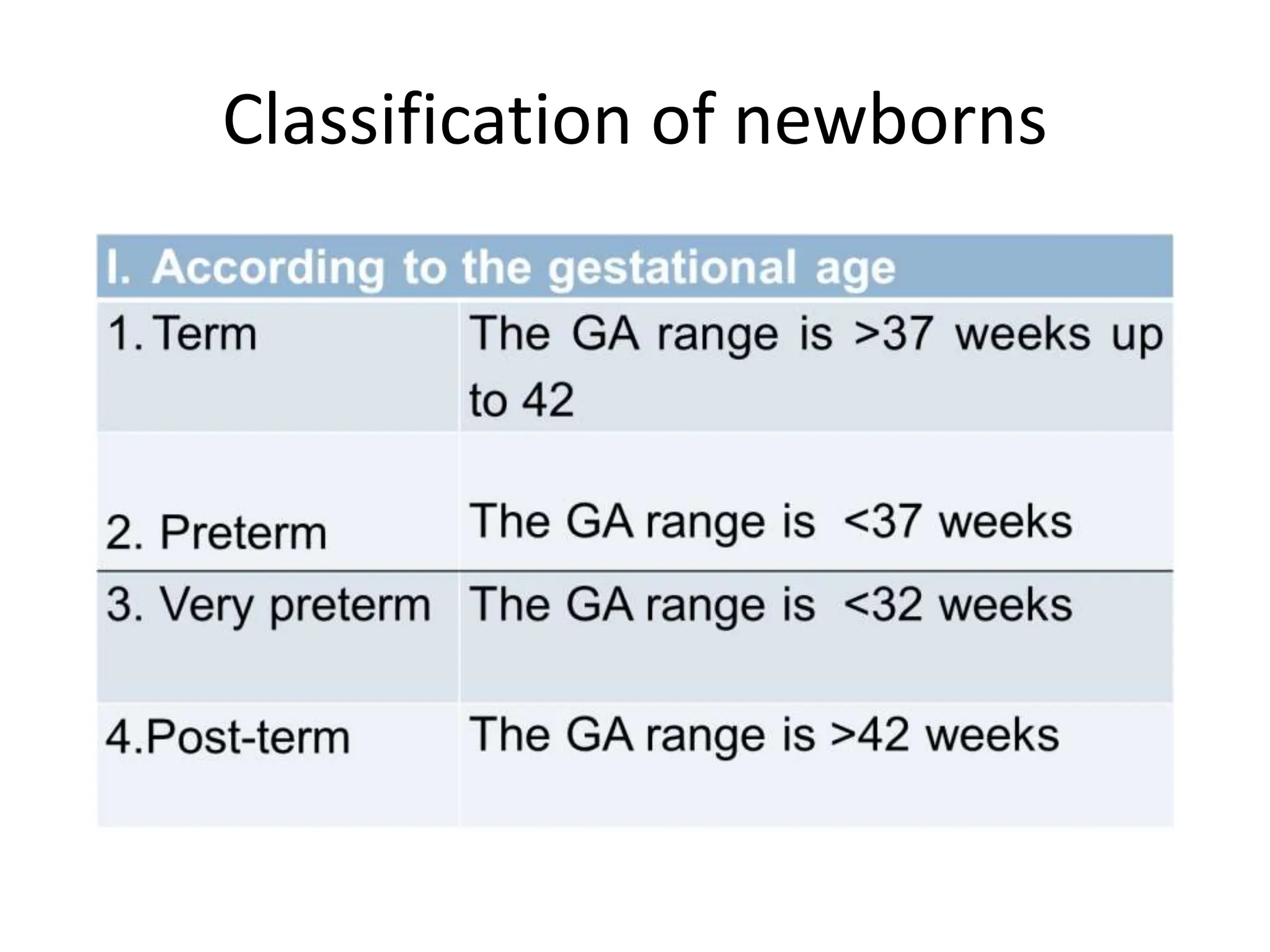
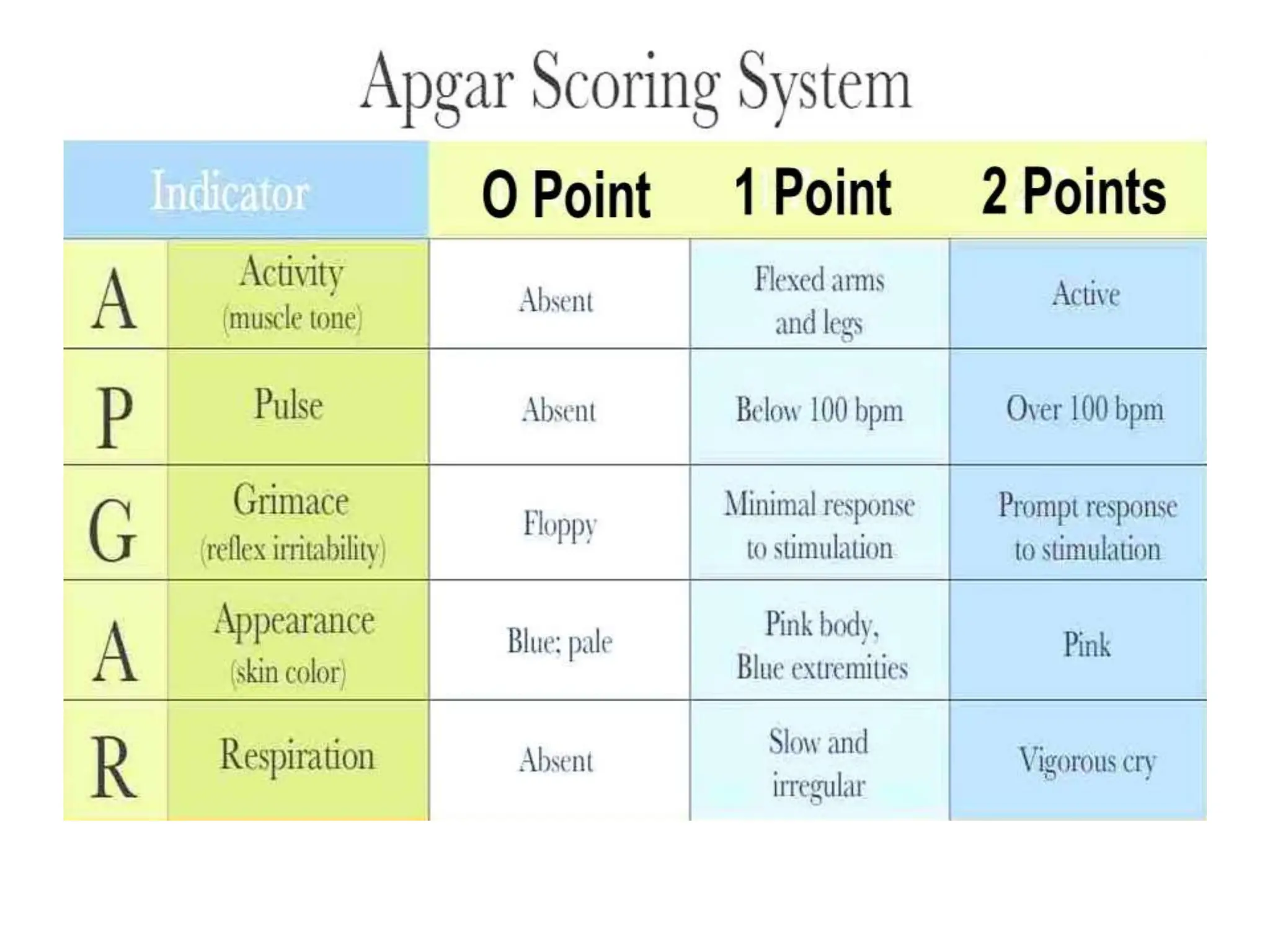
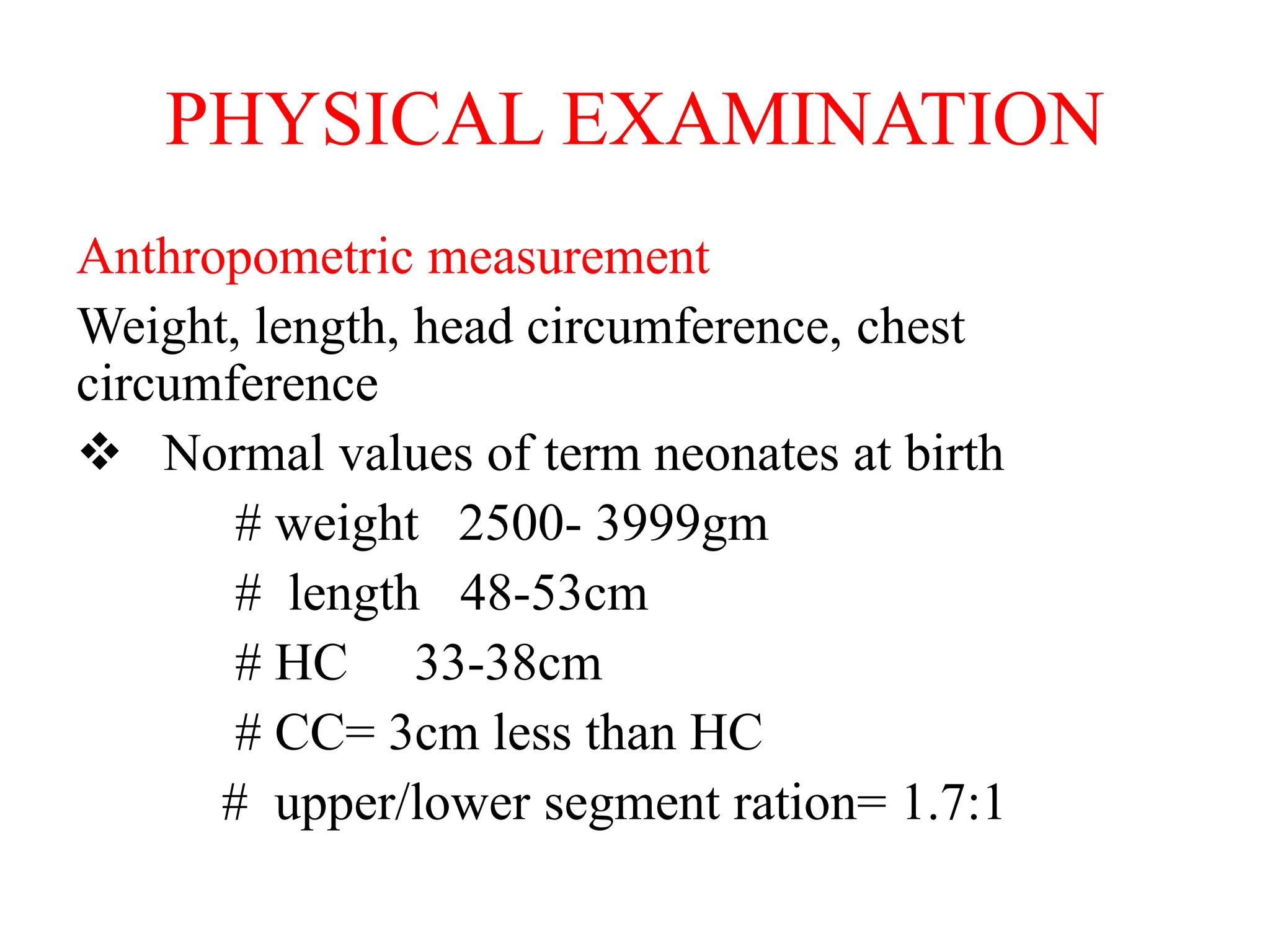
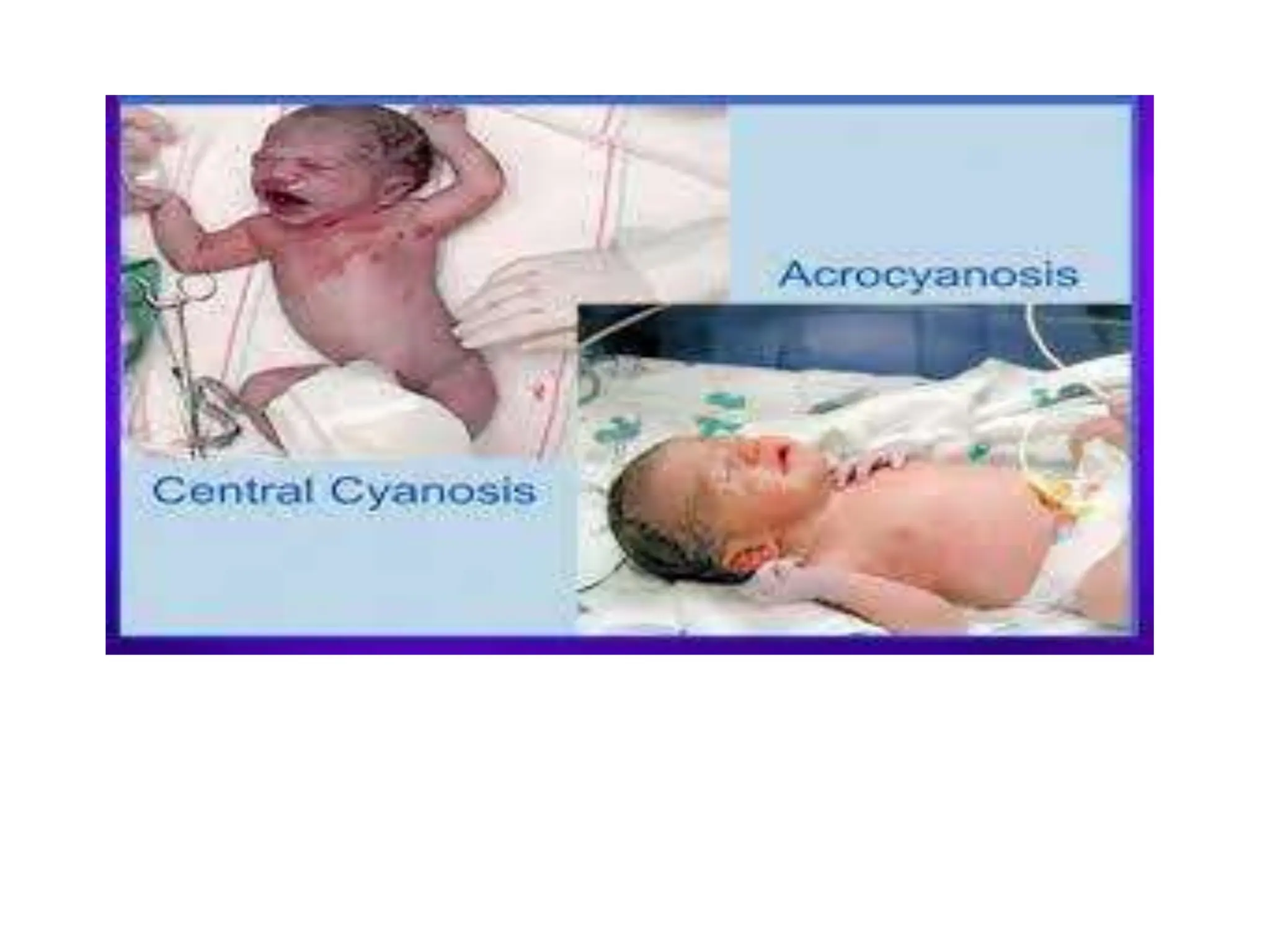
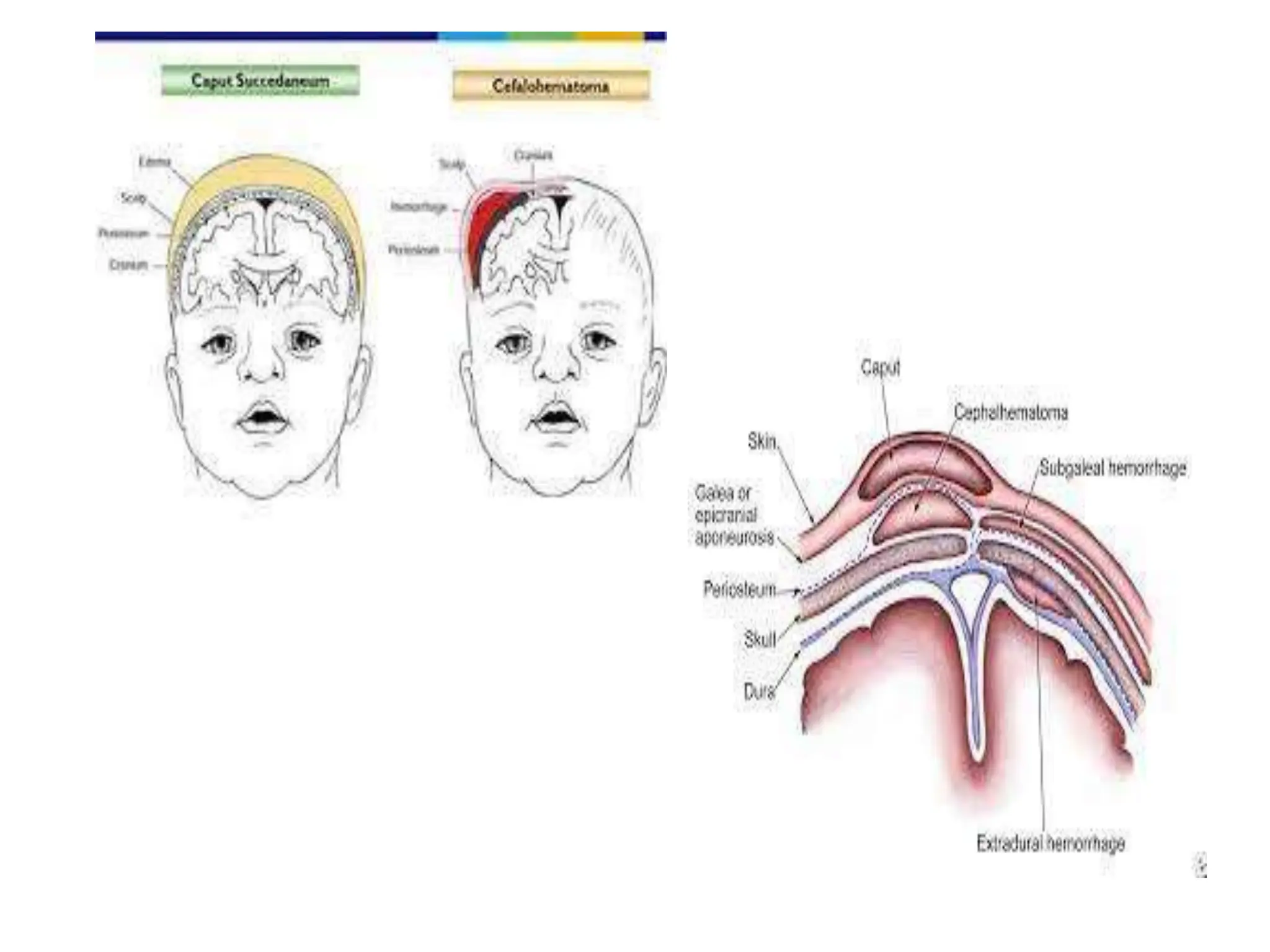
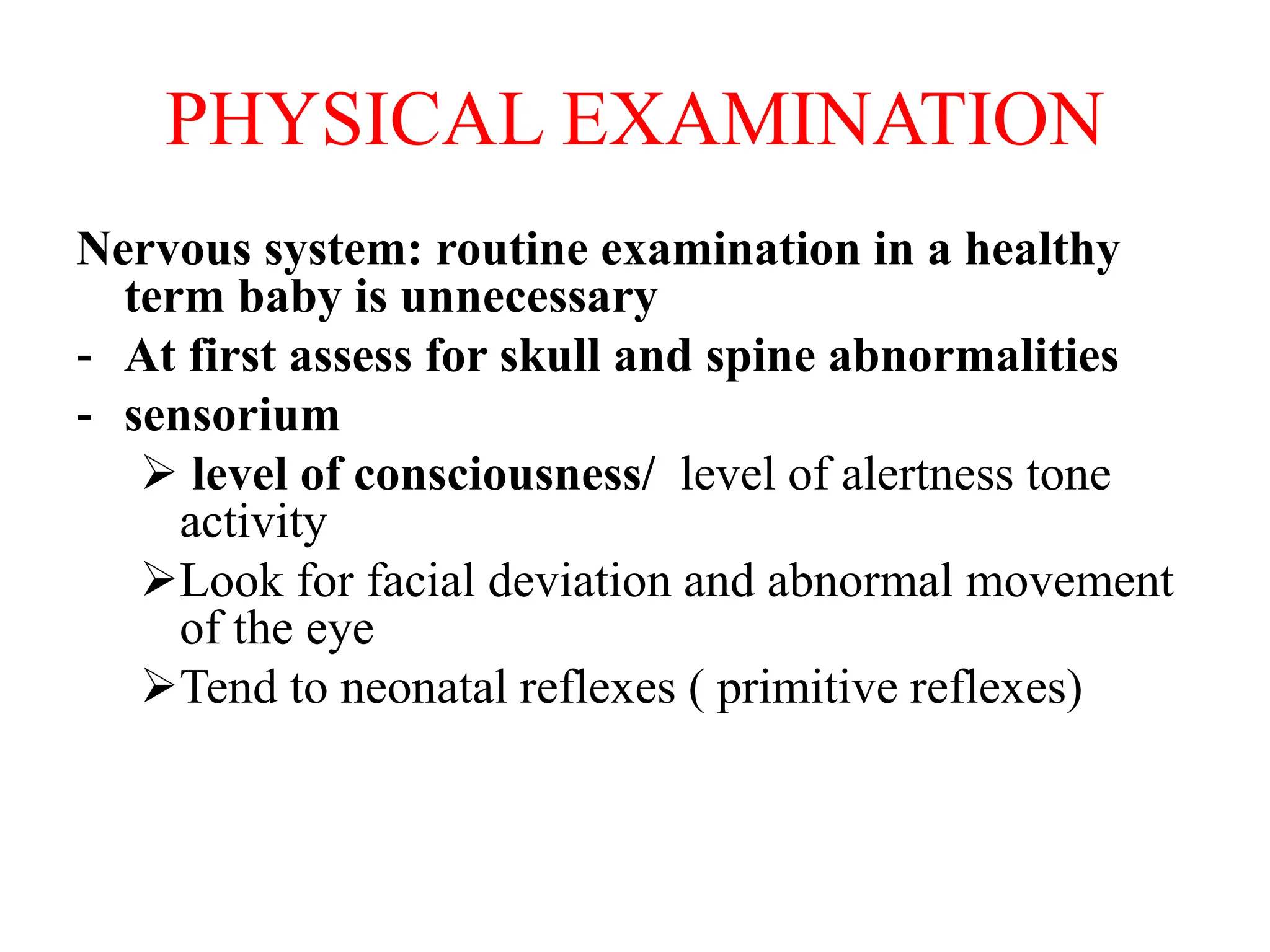
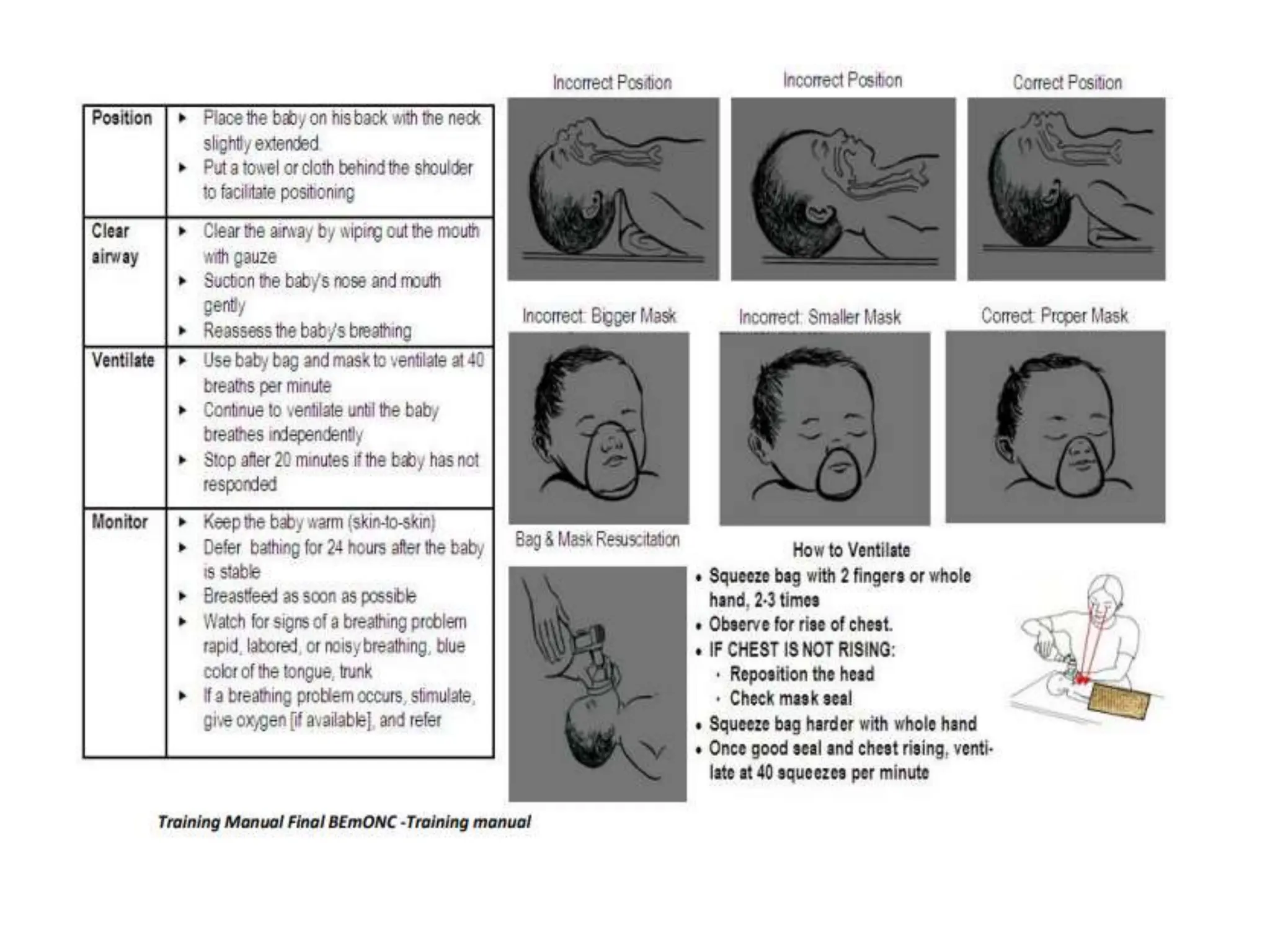
Neonatology is the branch of pediatrics that studies neonates, defined as infants from birth to 28 days of age. Essential newborn care includes 13 steps to support survival and wellbeing, such as drying the baby, checking breathing, clamping the umbilical cord, initiating skin-to-skin contact and breastfeeding within 1 hour, administering eye ointment and vitamin K, and recording observations. Routine newborn assessment evaluates breathing, muscle tone, skin color, temperature and other factors to identify issues requiring special care. The Apgar score is used to assess how well an infant tolerated birth and is adapting outside the womb, with points given in 5 categories at 1 and 5 minutes after