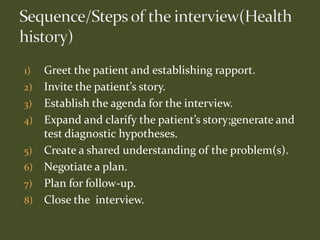
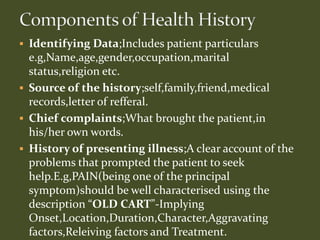
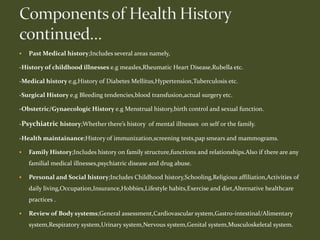
Taking a thorough medical history is essential for correctly diagnosing a patient's problem. The medical history involves acquiring information from the patient to form a diagnosis and provide appropriate care. It should be comprehensive, systematic, and follow established steps. Without a thorough understanding of the patient's history, their problems may remain undiagnosed despite physical exams and test results.