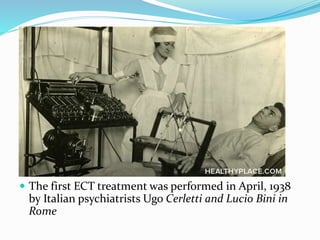
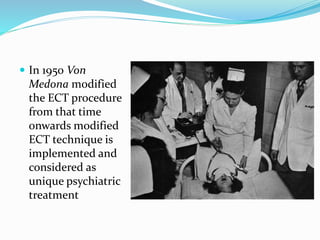
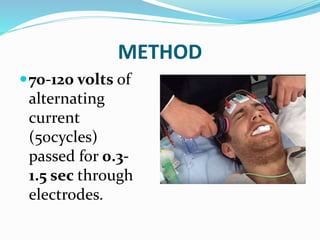
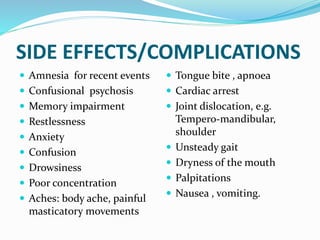
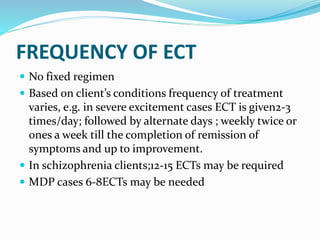
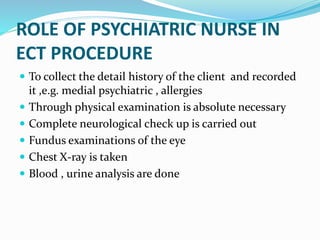
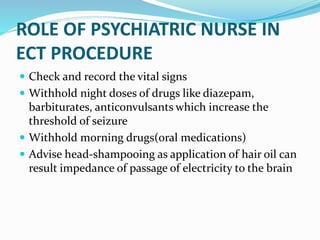
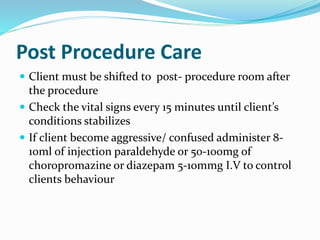
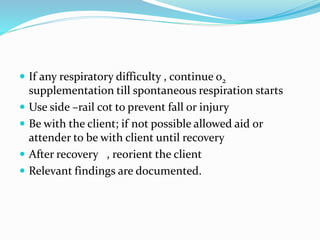
The document discusses the history and development of electroconvulsive therapy (ECT). It notes that ECT was first used in the 1500s using camphor, was modernized in the 1930s using camphor for catatonic schizophrenia, and the first official ECT treatment was in 1938 in Rome. It then describes the concept, definition, purpose, methods, mechanisms of action, types, applications of electrodes, techniques, ECT team, indications, contraindications, side effects, frequency, and the roles of psychiatric nurses in the ECT procedure.