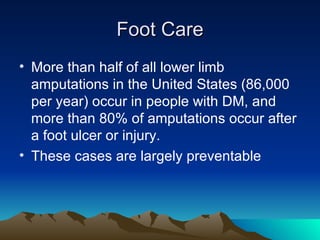
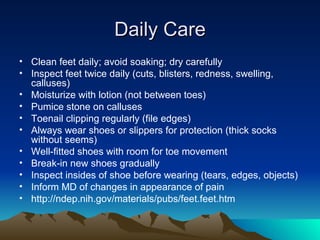
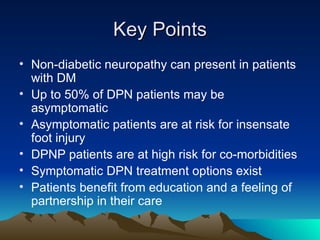
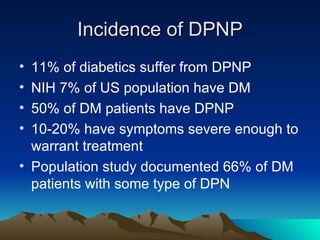
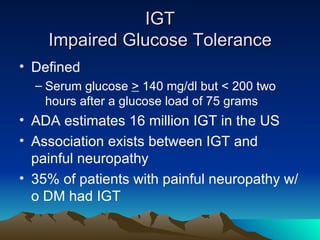
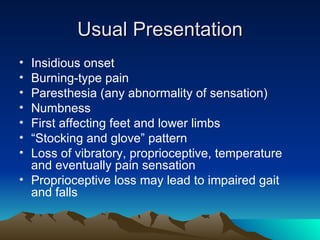
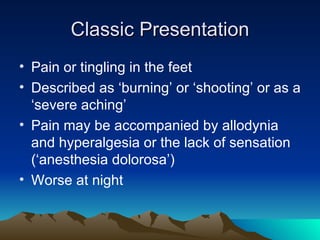
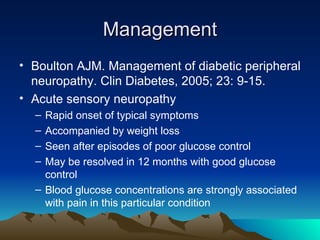
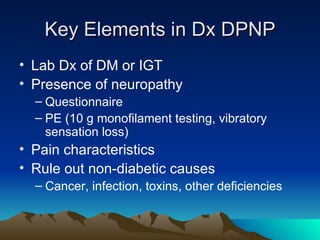
The document discusses recommendations for treating diabetic peripheral neuropathic pain (DPNP) created by a consensus group in 2005. It provides an overview of DPNP, including definitions, incidence rates, assessment tools, management guidelines, and recommendations for first- and second-tier medication treatments. It also covers the typical clinical presentation of DPNP and importance of foot care to prevent ulcers and amputations.

![Second-Tier Medications Anticonvulsants Carbamazepine (Tegretol) Gabapentin (Neurontin) Lamotragine (Lamictal) Tramadol (Ultram) Venlafaxine (Effexor) [extended release]](https://image.slidesharecdn.com/dpnp-124301394567-phpapp01/85/DPNP-6-320.jpg)
![10 g monofilament Semmes-Weinstein 10 gram monofilament Nylon filament bends at 10 g force applied Toe and 1 st , 3 rd and 5 th metatarsal heads Predicts feet at risk for ulcerations with 86% – 100% sensitivity (TP/TP+FN) [identifying those with disease]](https://image.slidesharecdn.com/dpnp-124301394567-phpapp01/85/DPNP-19-320.jpg)