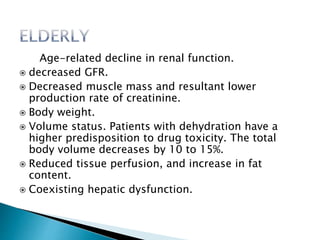
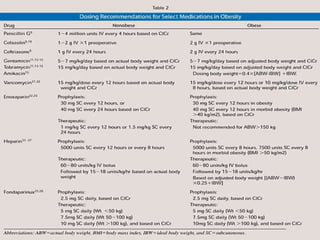
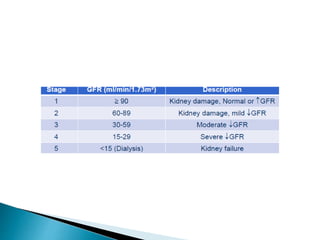
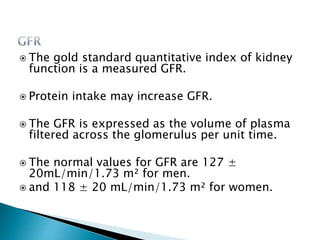
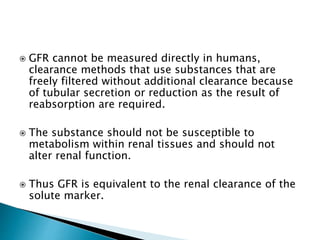
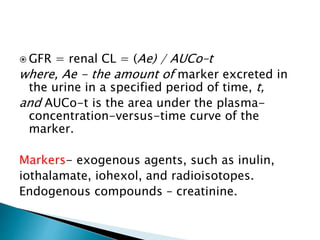
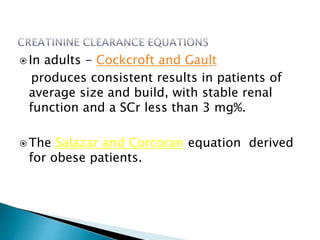
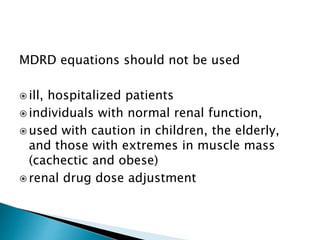
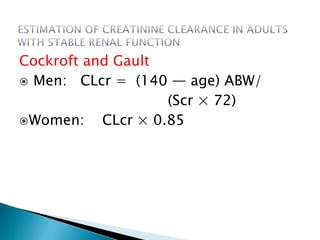
The document provides an overview of kidney functions and pharmacokinetic changes in patients with chronic kidney disease (CKD), discussing drug elimination, absorption, and effects on drug metabolism. It emphasizes the importance of estimating glomerular filtration rate (GFR) using various equations for adjusting drug dosages in renal insufficiency. The document includes detailed calculations and considerations for different patient populations, including children and the elderly.
![ For the estimation of GFR.
six-variable Modification of Diet in Renal Disease
Study (MDRD6) equation:
GFR = 170 × (Pcr)-0.999 × [Age]-0.176 ×
[0.762 if patient is female] ×
[1.180 if patient is black] ×
[SUN]-0.170 × [Alb]-0.318
where , Pcr = plasma creatinine,
SUN = serum nitrogen concentration,
and Alb = serum albumin concentration.](https://image.slidesharecdn.com/doseadjustmentinrenaldisorder-190329054005/85/Dose-adjustment-in-renal-disorder-16-320.jpg)
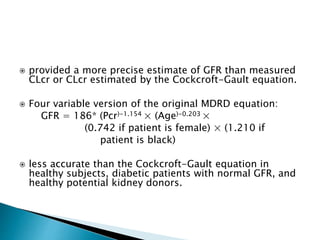
![Renal function does not mature to reach adult
values until one year of age.
rapid changes in GFR.
Estimation of CLcr - Schwartz is dependent on the
child’s age and length:
GFR = [length (cm) × k] / Scr
where, k is defined by age group:
pre-term infants = 0.33
infant (1 to 52 weeks) = 0.45;
child(1 to 13 years) = 0.55;
adolescent male = 0.7;
and adolescent female= 0.55.](https://image.slidesharecdn.com/doseadjustmentinrenaldisorder-190329054005/85/Dose-adjustment-in-renal-disorder-20-320.jpg)