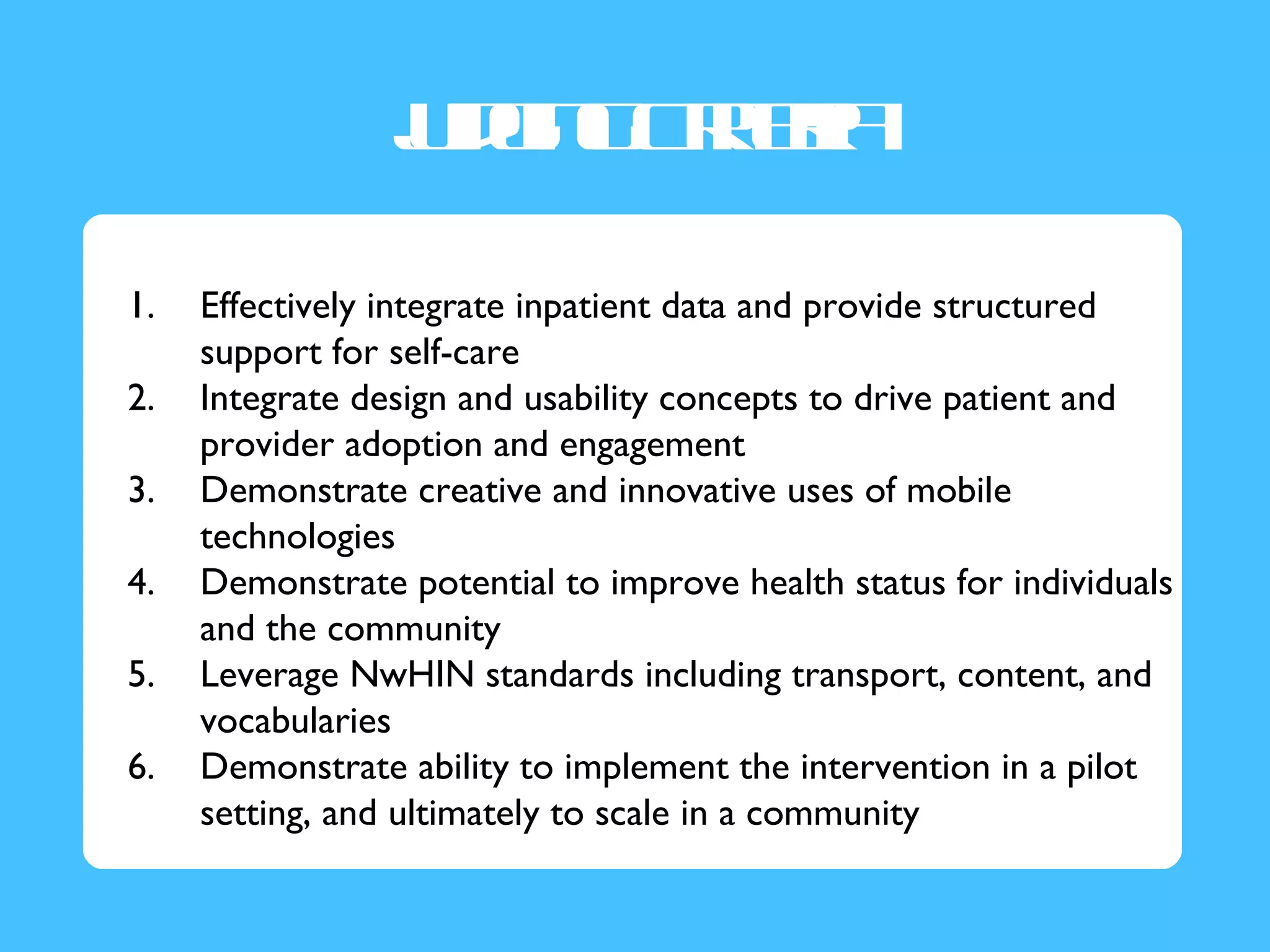
The document summarizes a webinar presentation on discharge follow-up appointments and care transitions. It provides an overview of the Office of the National Coordinator's i2 program which aims to spur innovation and highlight excellence. It then discusses the problem of care transitions and the opportunity to improve follow-up appointments. The document outlines elements of high-quality transitions and impacts on patients. It introduces the Critical Transitions Challenge to create a tool to improve post-discharge scheduling. It provides details on the challenge including desired tool components, pilot planning advice, and judging criteria.