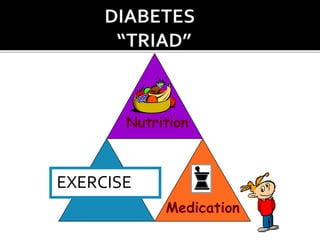
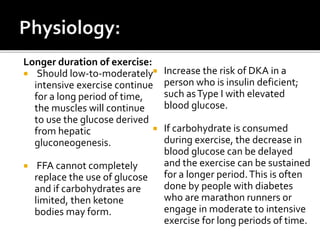
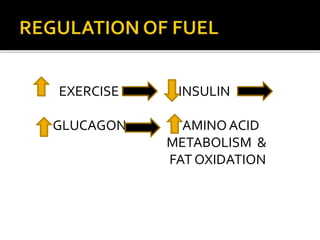
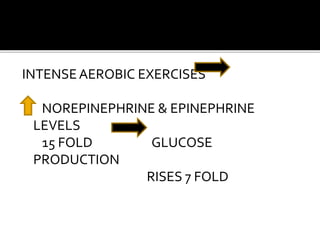
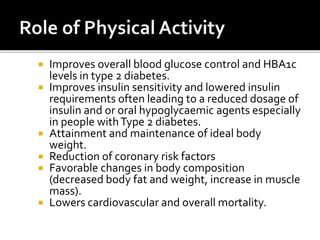
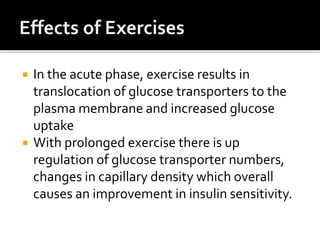
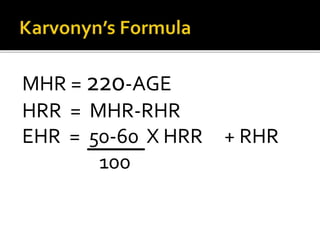
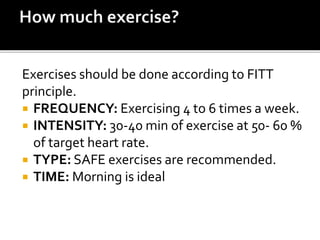
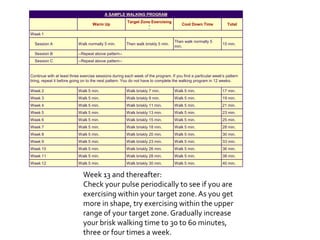
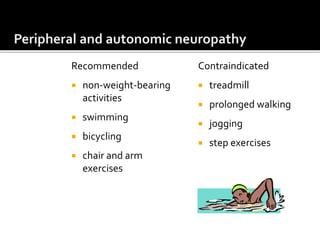
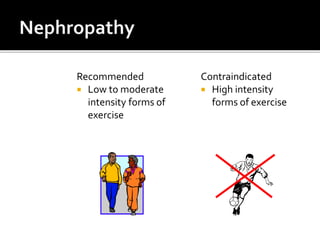
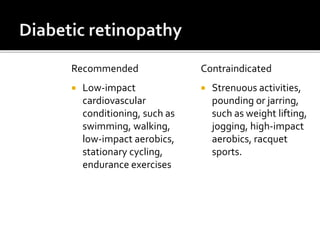
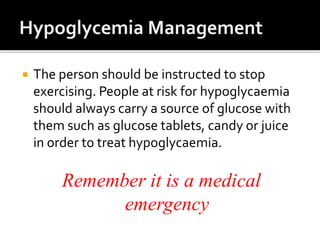
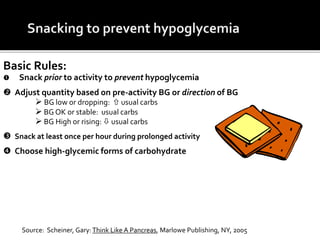
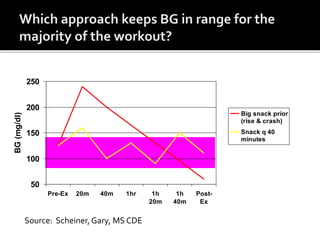
The document outlines the role of exercise in managing diabetes, emphasizing its efficacy in improving insulin sensitivity and blood glucose control. It details the physiological changes during different exercise durations and the necessity of carbohydrate intake during prolonged activity. Additionally, it provides guidelines for safe exercise practices tailored for individuals with diabetes, alongside recommendations for both aerobic and anaerobic exercises.