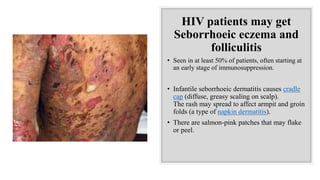
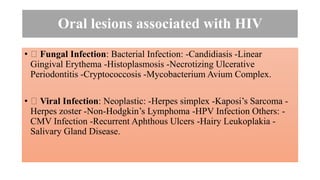
This document discusses various skin lesions and oral manifestations that can occur due to viral, bacterial, fungal infections and autoimmune diseases.
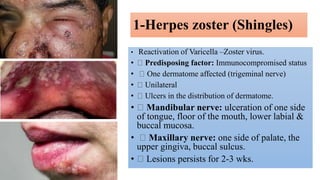
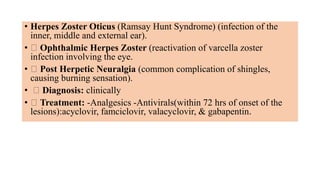
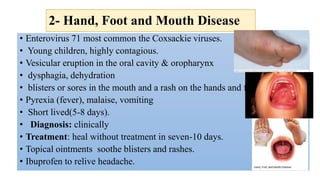
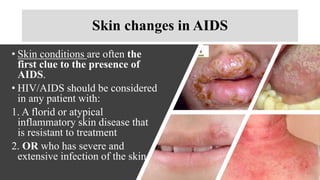
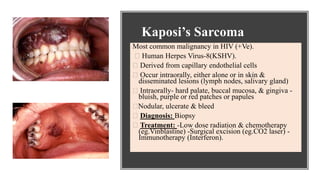
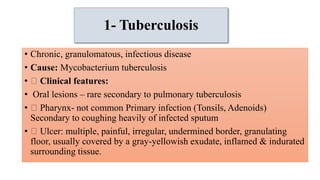
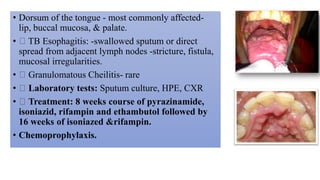
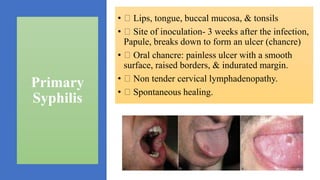
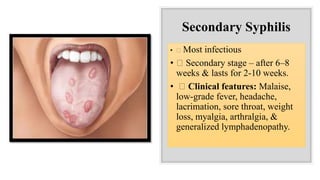
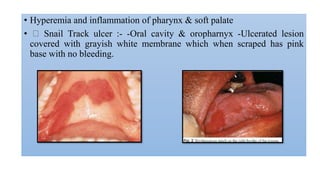
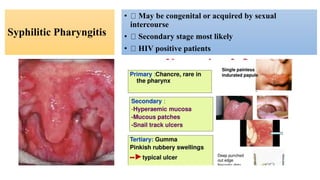
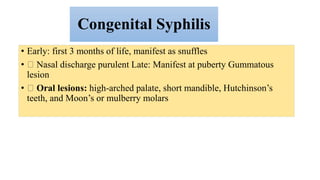
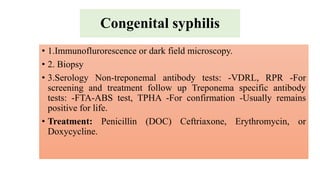
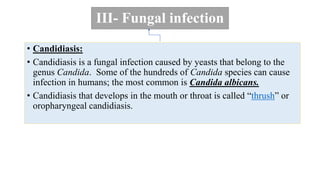
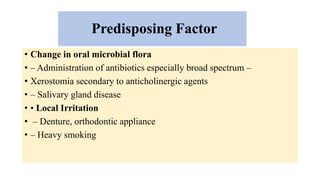
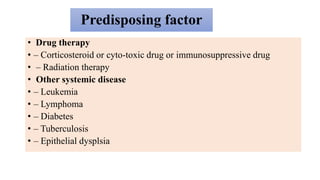
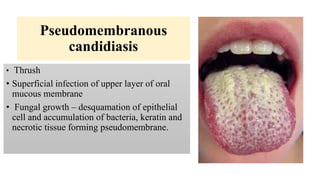
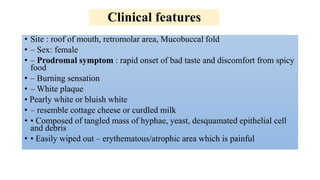
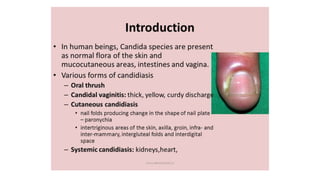
It provides details on Herpes Zoster (Shingles), Hand Foot and Mouth disease caused by viruses. Bacterial infections like Tuberculosis and Syphilis are explained. Candidiasis is discussed as the common fungal infection causing thrush in the oral cavity. Skin conditions and oral lesions associated with HIV/AIDS are summarized. Treatment options for many of these conditions are also mentioned.