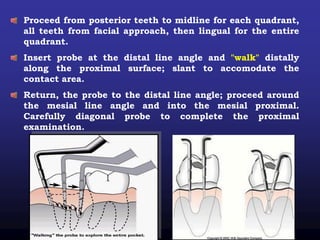
This document discusses the importance of dental charting for documenting a patient's periodontal condition. It describes how to record details of the gingiva such as color, size, shape and texture. It also provides guidance on charting probing depths, bleeding, exudate, recession, furcation involvement, plaque, calculus, and tooth mobility. Maintaining accurate dental charts is essential for establishing diagnoses, treatment plans and monitoring a patient's response to periodontal therapy over time.