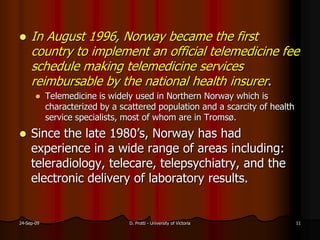
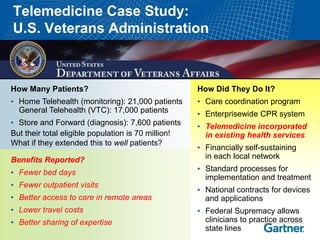
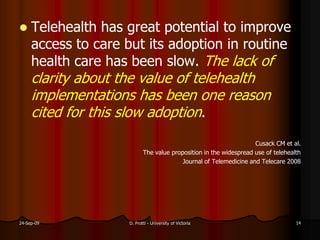
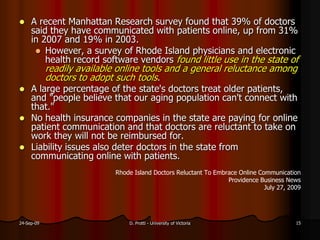
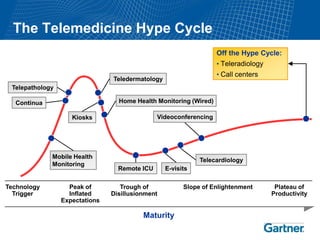
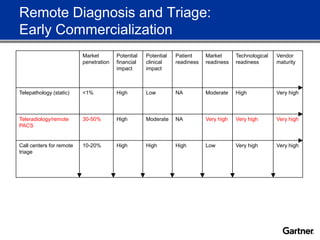
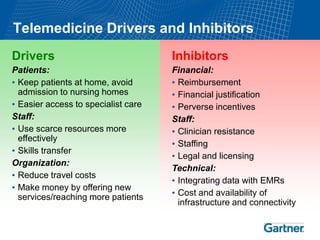
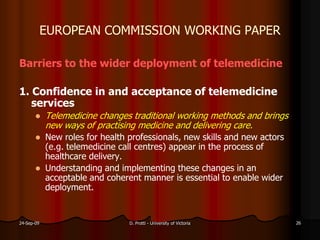
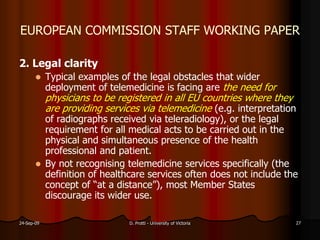
This document summarizes a presentation on assessing and enhancing the public value of telehealthcare. It begins by discussing the various terms used in telehealth, including telehealthcare, telemedicine, telecare, telemonitoring, and eHealth. It then reviews definitions of telemedicine from Cochrane reviews, the European Commission, and other sources. The presentation notes the potential benefits of telehealthcare, such as reduced hospital and care home days, but also discusses challenges to adoption like a lack of clarity around cost savings and reluctance from physicians.