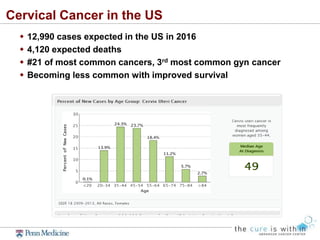
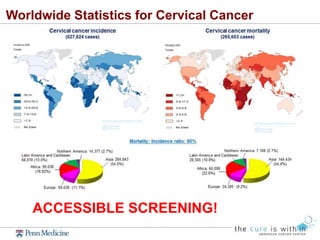
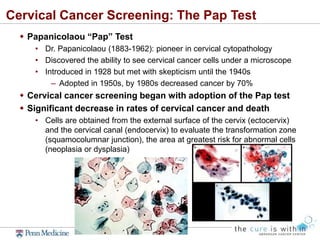
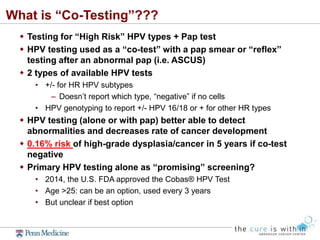
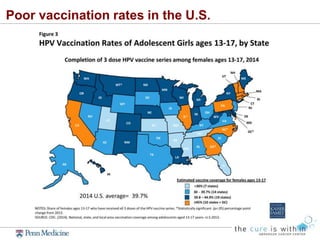
This document summarizes gynecologic cancer screening recommendations presented by Dr. Ashley Haggerty. It discusses screening guidelines for cervical cancer using Pap tests and HPV testing, noting a shift to less frequent screening. It also covers HPV vaccination and notes its effectiveness in preventing cervical cancer. For ovarian cancer, the document indicates screening is not currently recommended due to lack of evidence showing reduced mortality. It concludes by discussing debates around annual pelvic exams.