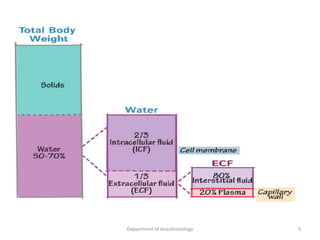
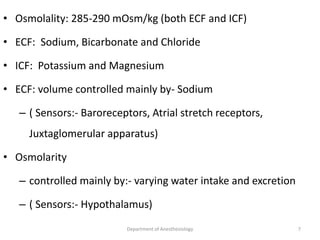
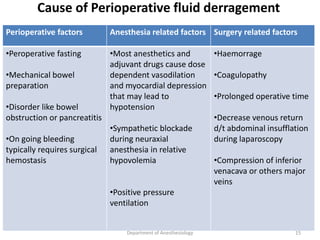
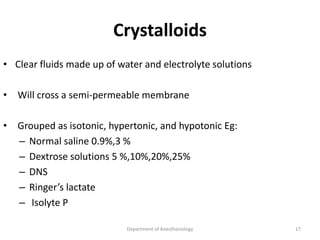
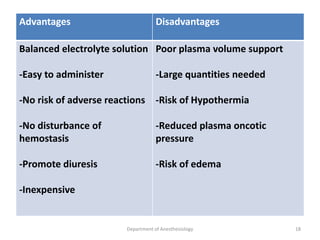
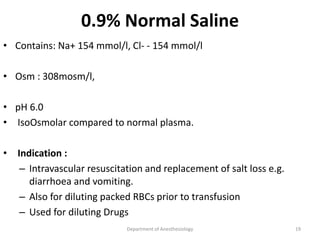
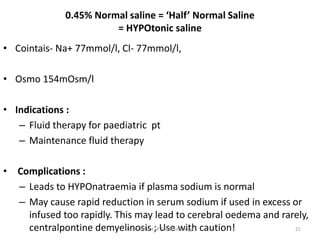
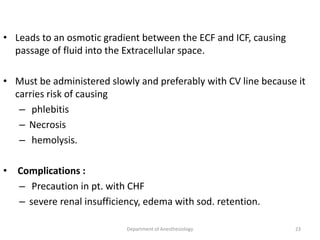
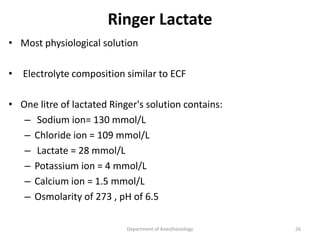
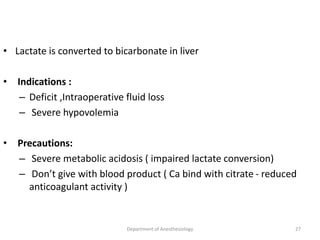
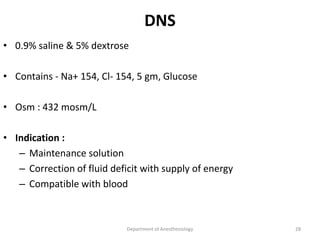
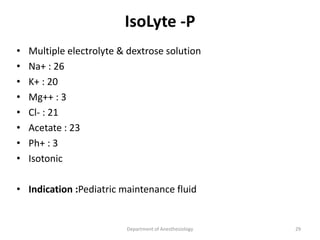
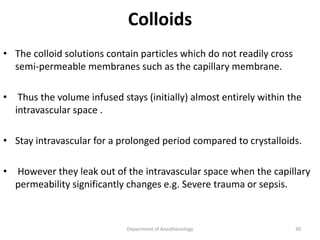
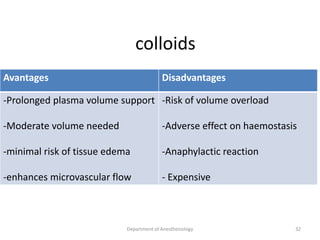
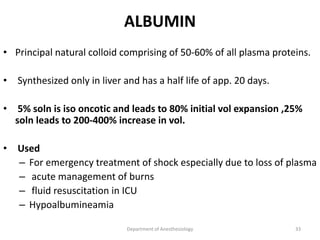
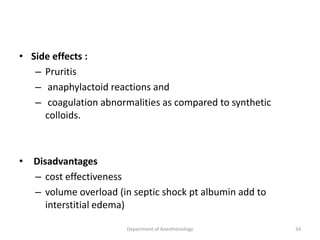
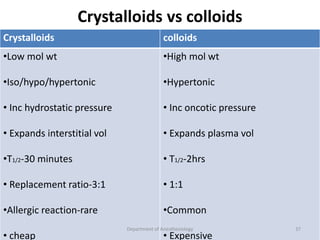
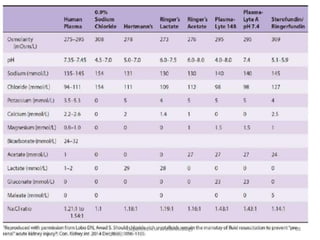
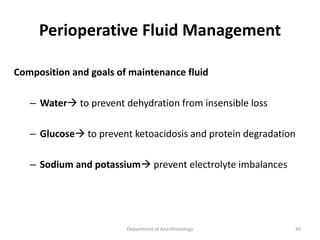
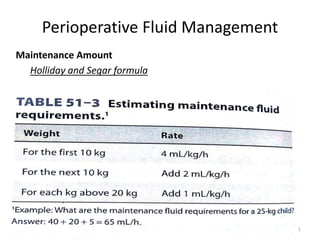
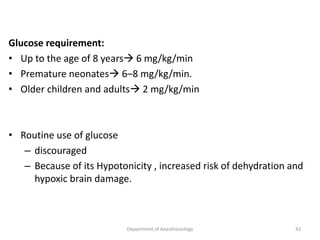
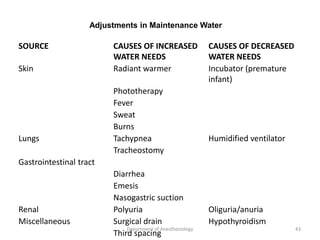
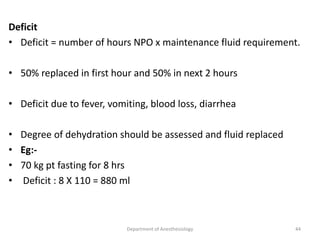
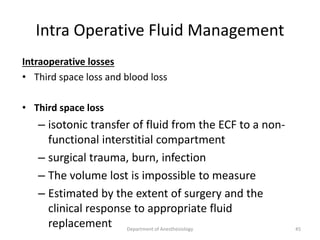
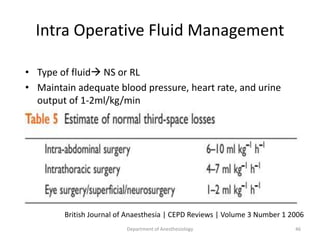
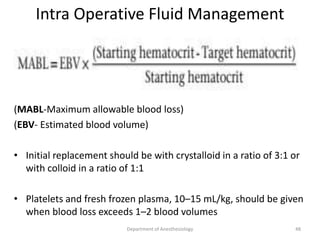
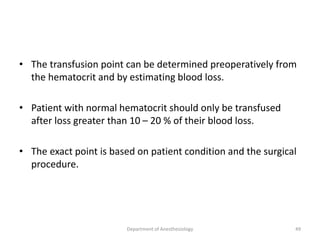
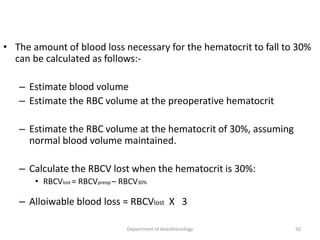
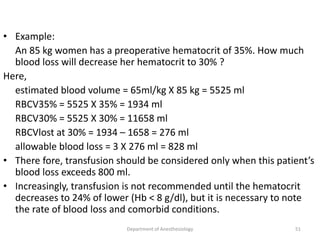
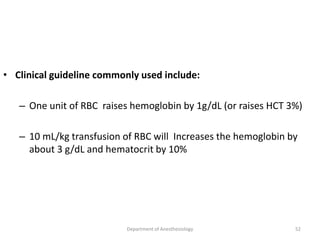
The document provides an overview of perioperative fluid therapy, focusing on the importance of fluid management to prevent dehydration and maintain adequate circulation and tissue perfusion. It discusses types of fluids (crystalloids and colloids), their indications, advantages, and disadvantages, as well as guidelines for fluid replacement during surgery. Additionally, it covers assessment techniques for intravascular volume and strategies for intraoperative fluid management, emphasizing the need for careful monitoring and tailored fluid administration.