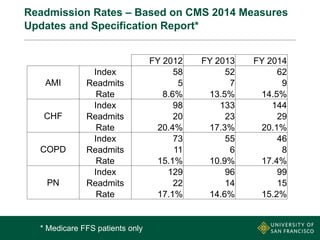
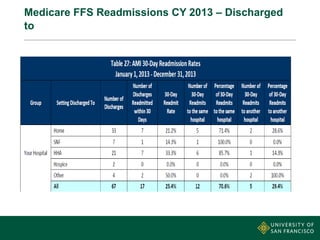
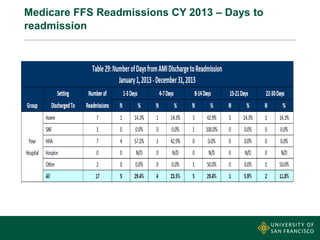
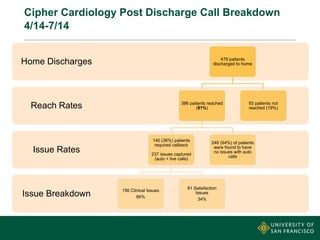
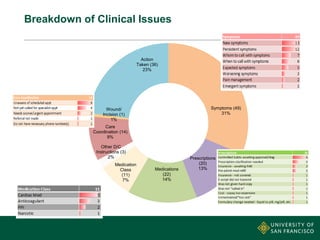
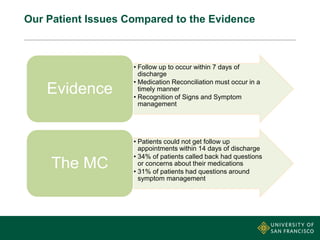
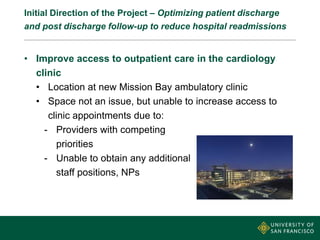
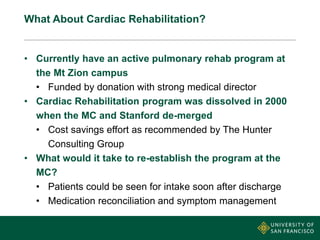
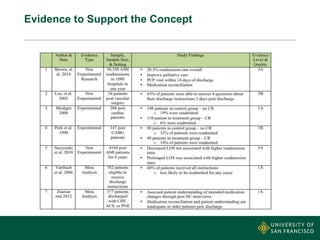
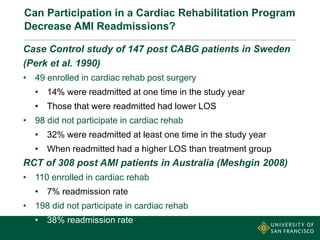
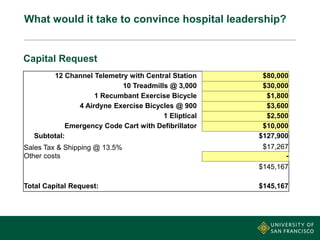
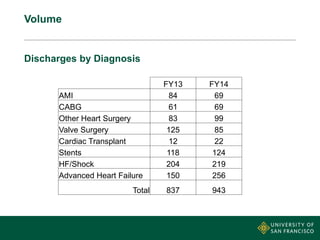
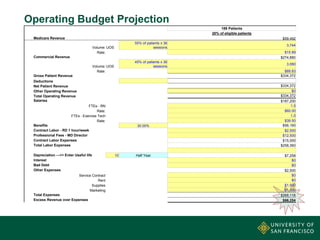
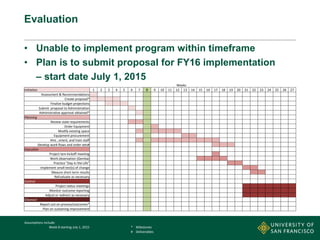
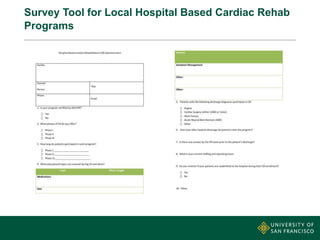
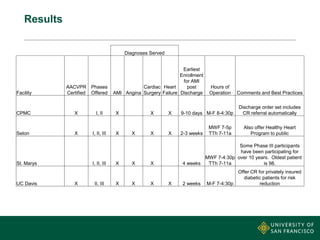
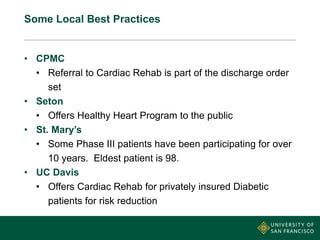
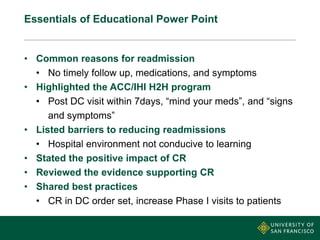
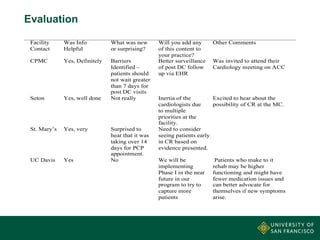
This document summarizes a presentation on avoiding 30-day readmissions of acute myocardial infarction (AMI) patients through the use of cardiac rehabilitation. It discusses the current high readmission rates at the medical center and initiatives to reduce them. The presentation evaluates starting a cardiac rehabilitation program, citing evidence it can decrease AMI readmissions. It includes a proposed budget and timeline. Surveys of local cardiac rehab programs found they reduced readmissions and shared best practices, such as automatically referring patients to rehab at discharge. An educational intervention for facilities highlighted barriers to reducing readmissions and evidence supporting cardiac rehab. Facilities found the information helpful and were interested in applying aspects to their own practices.