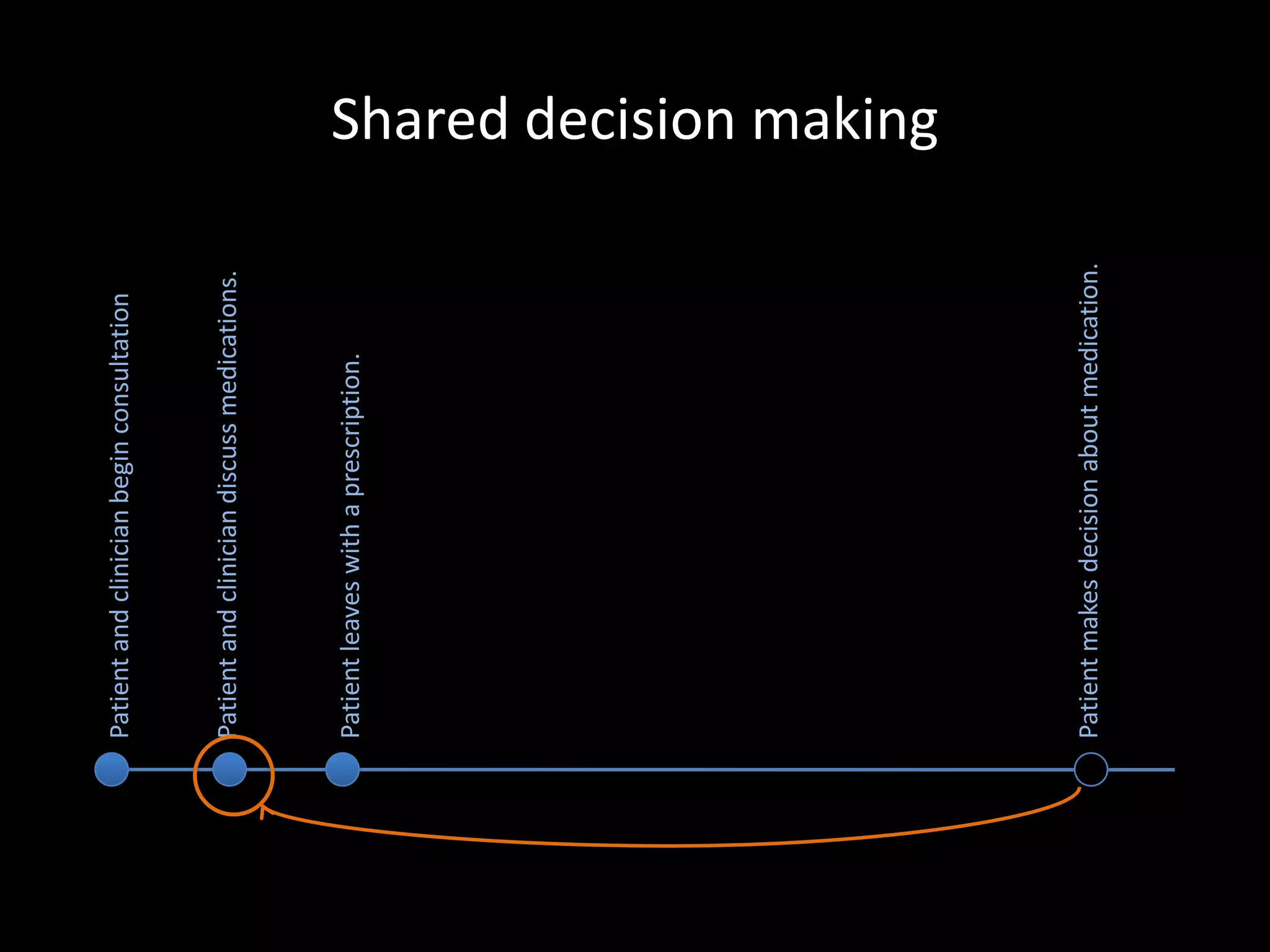
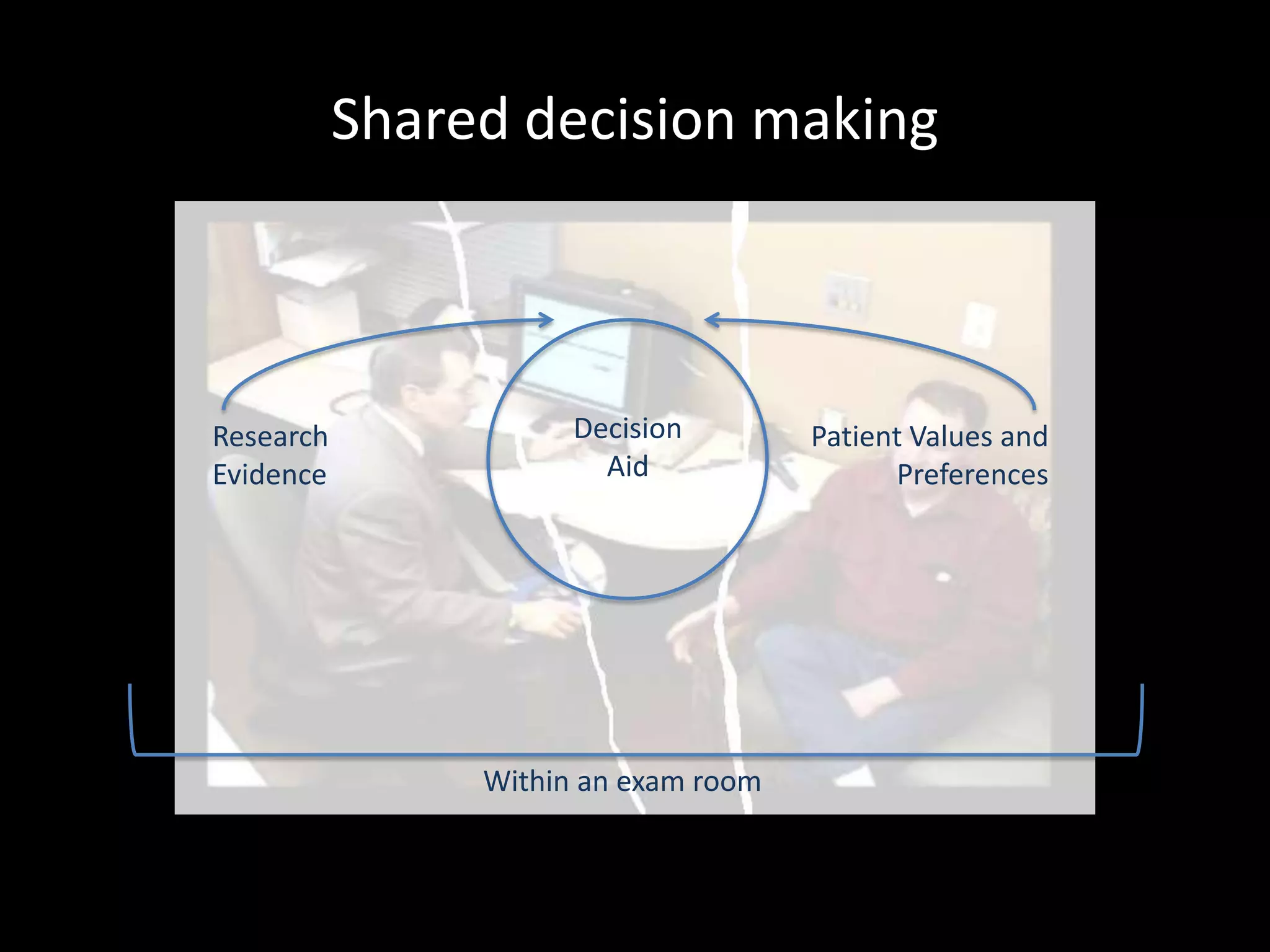
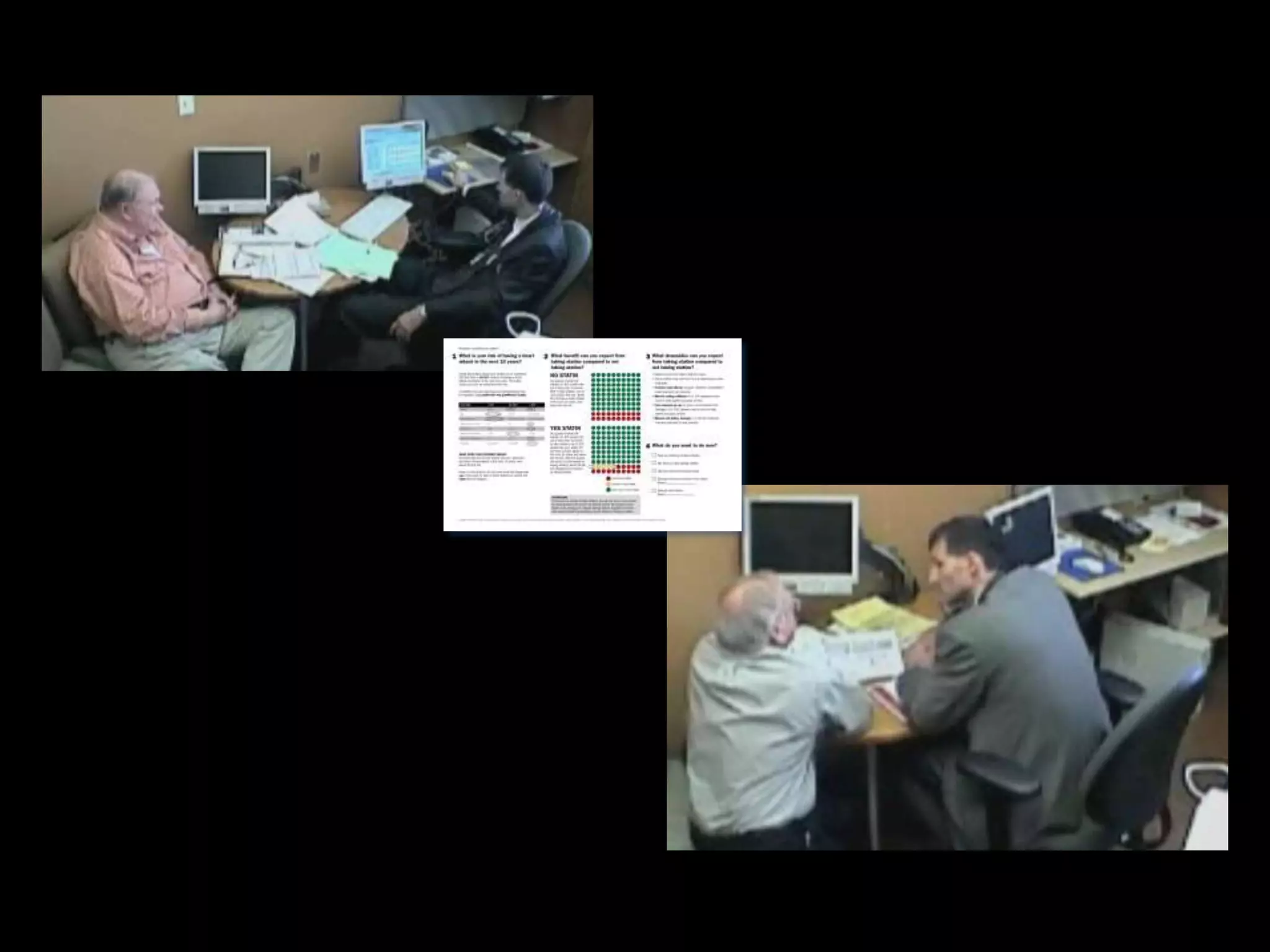
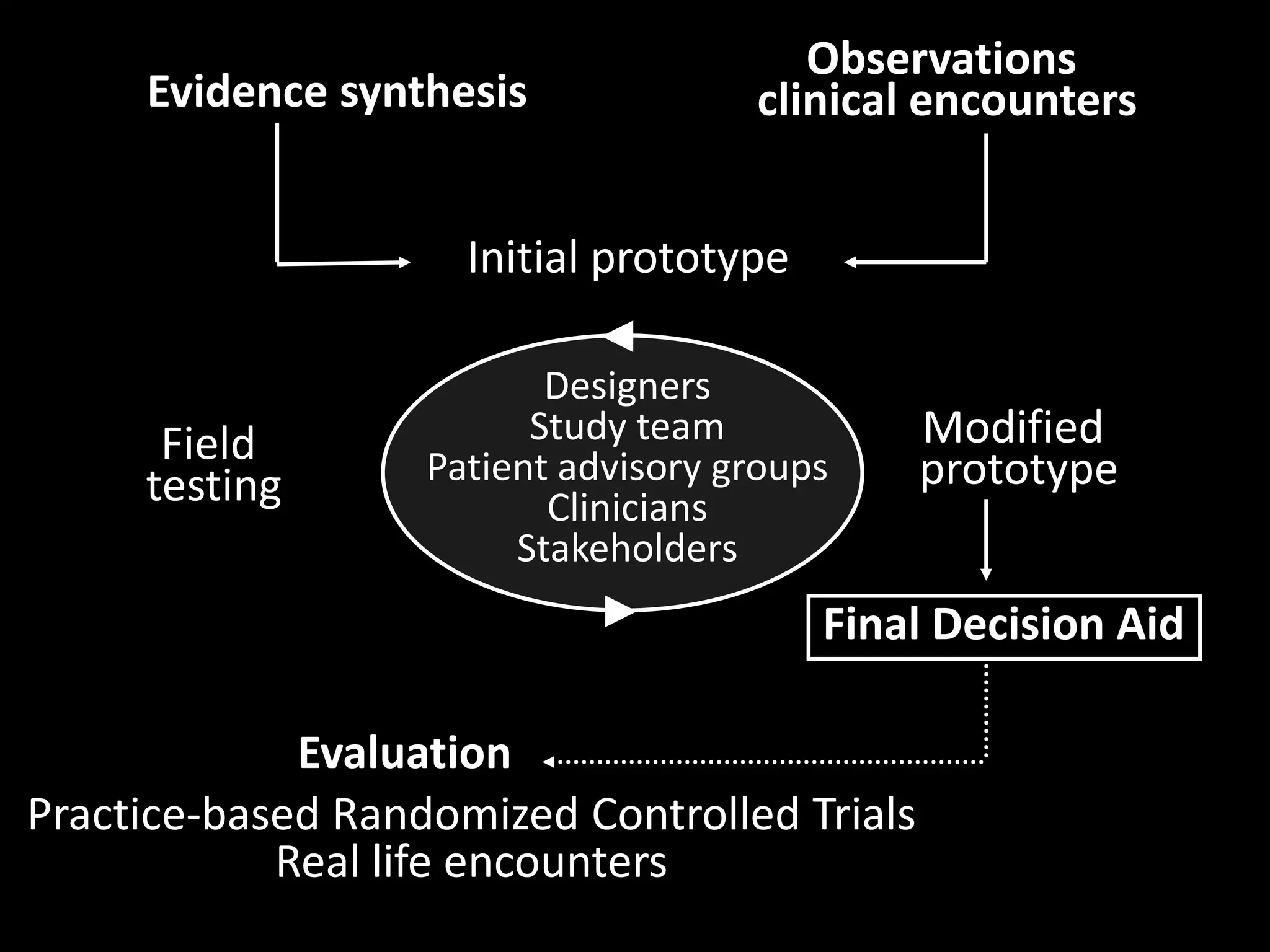
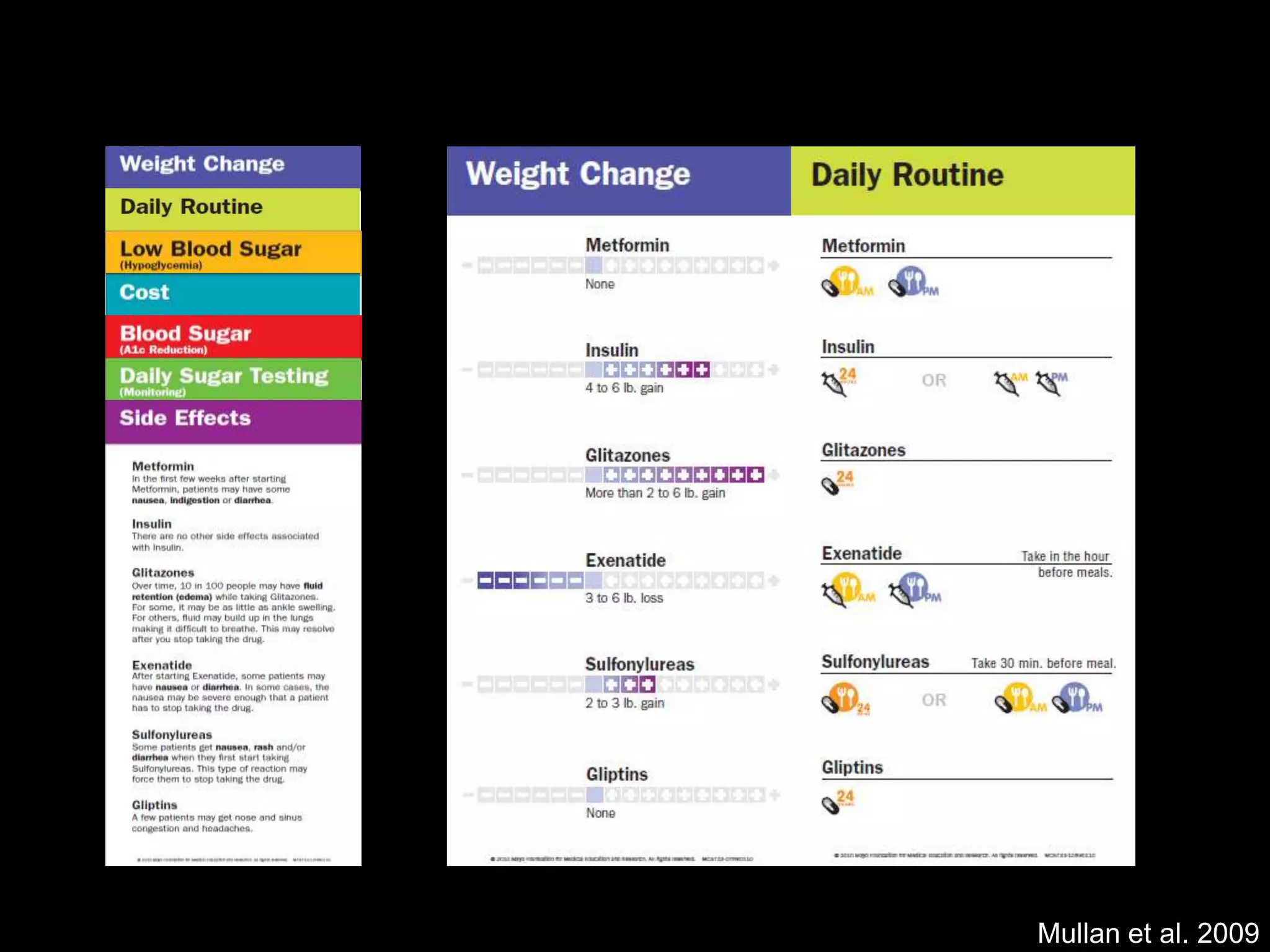
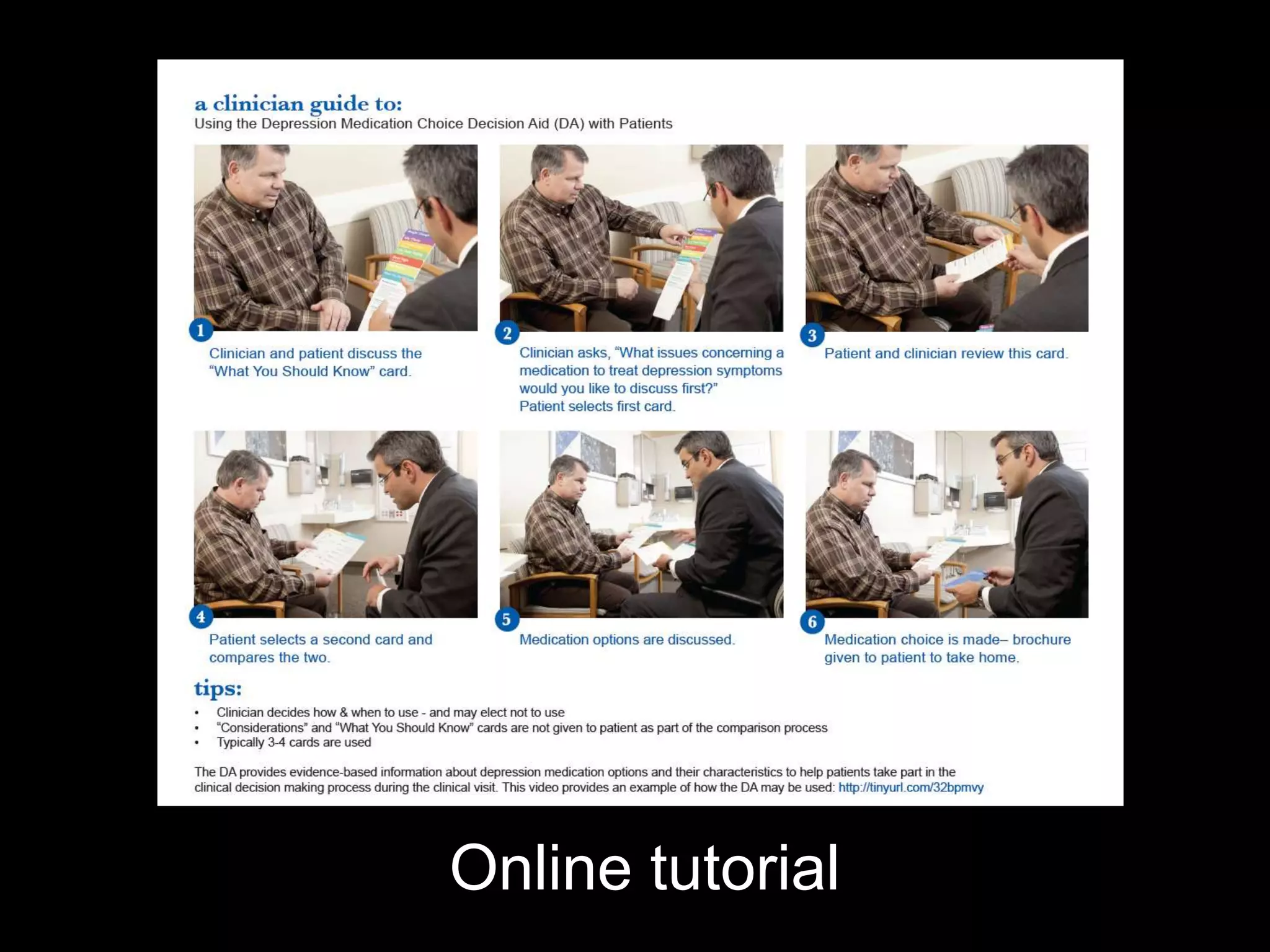
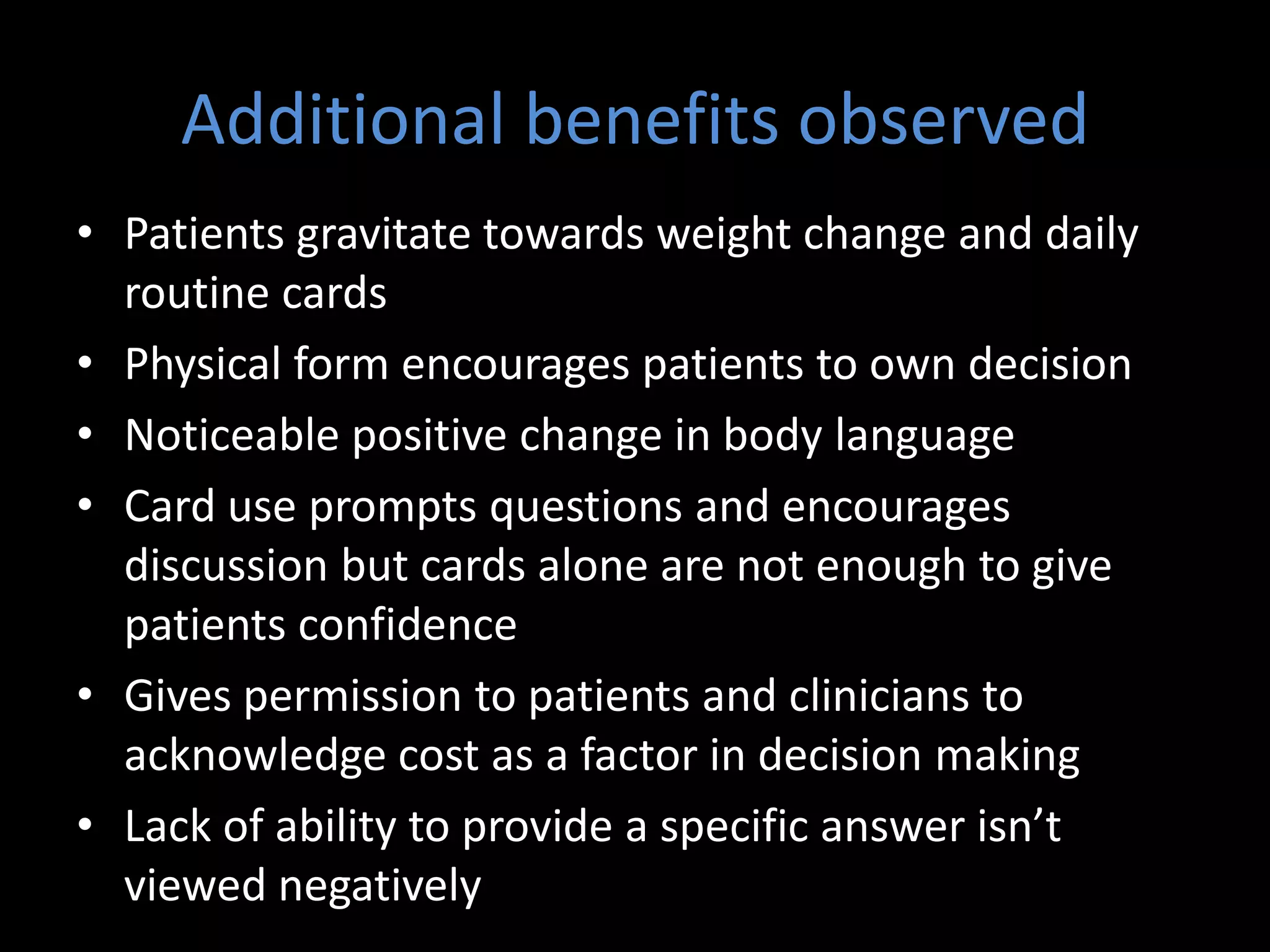
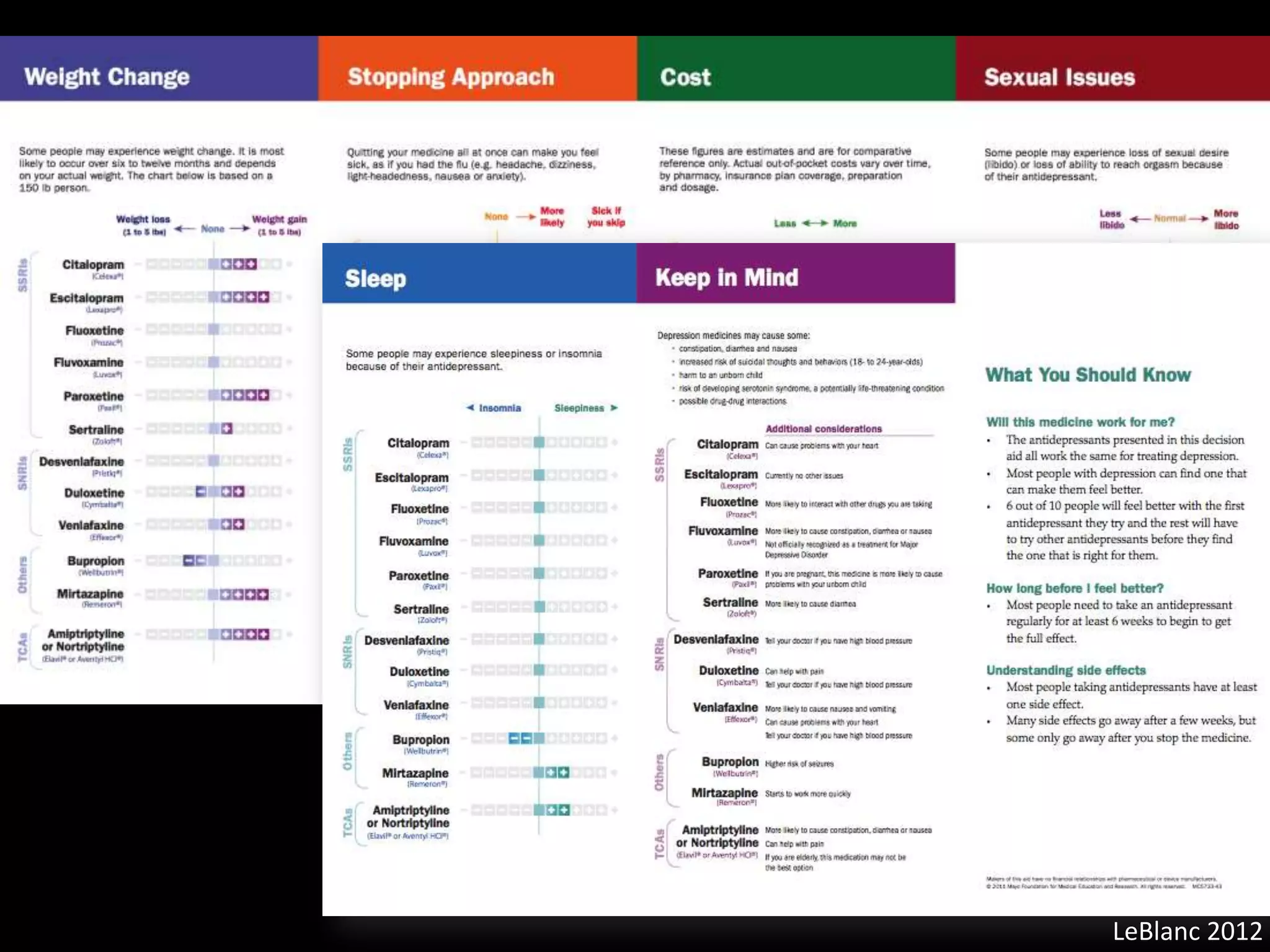
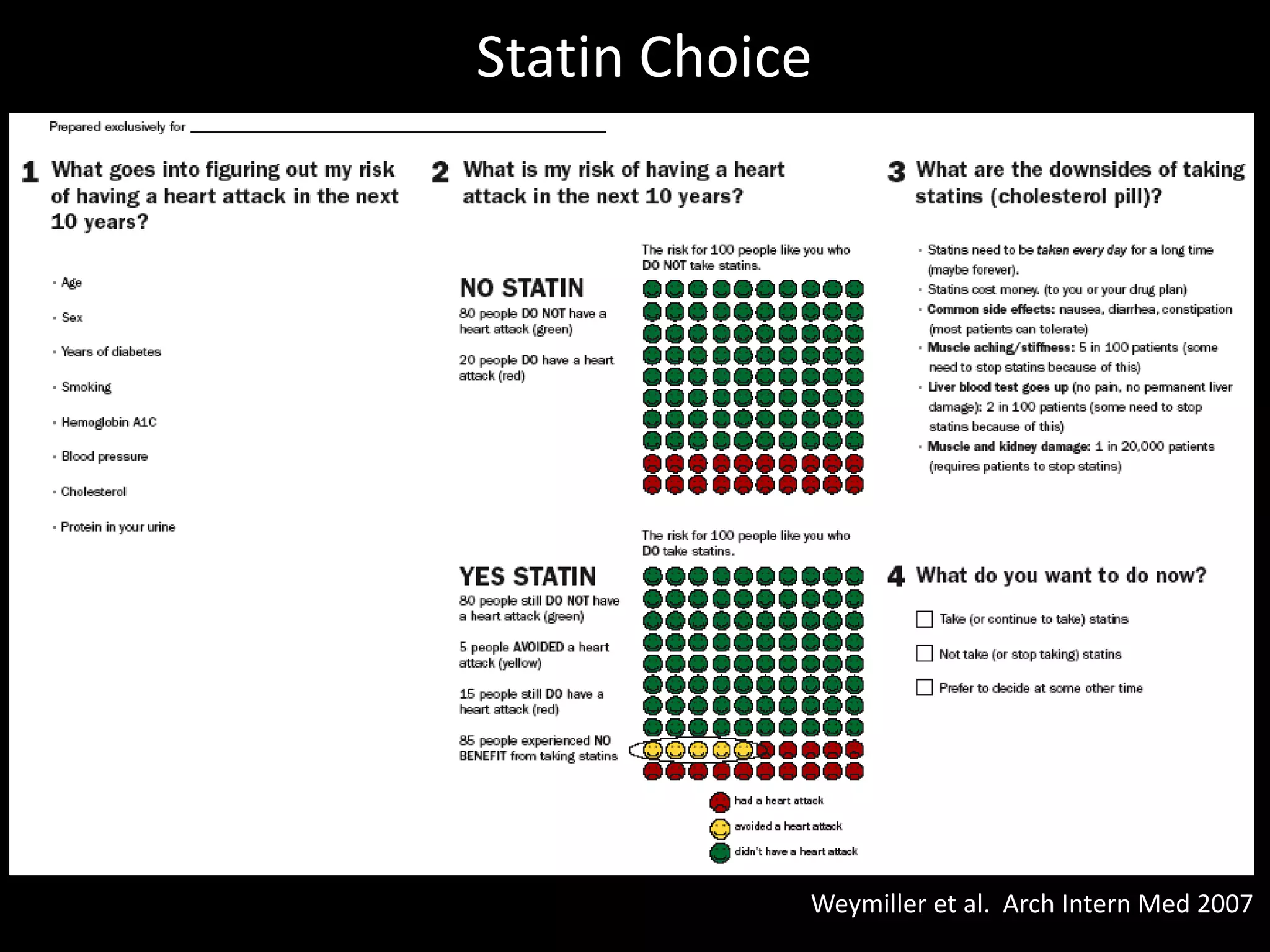
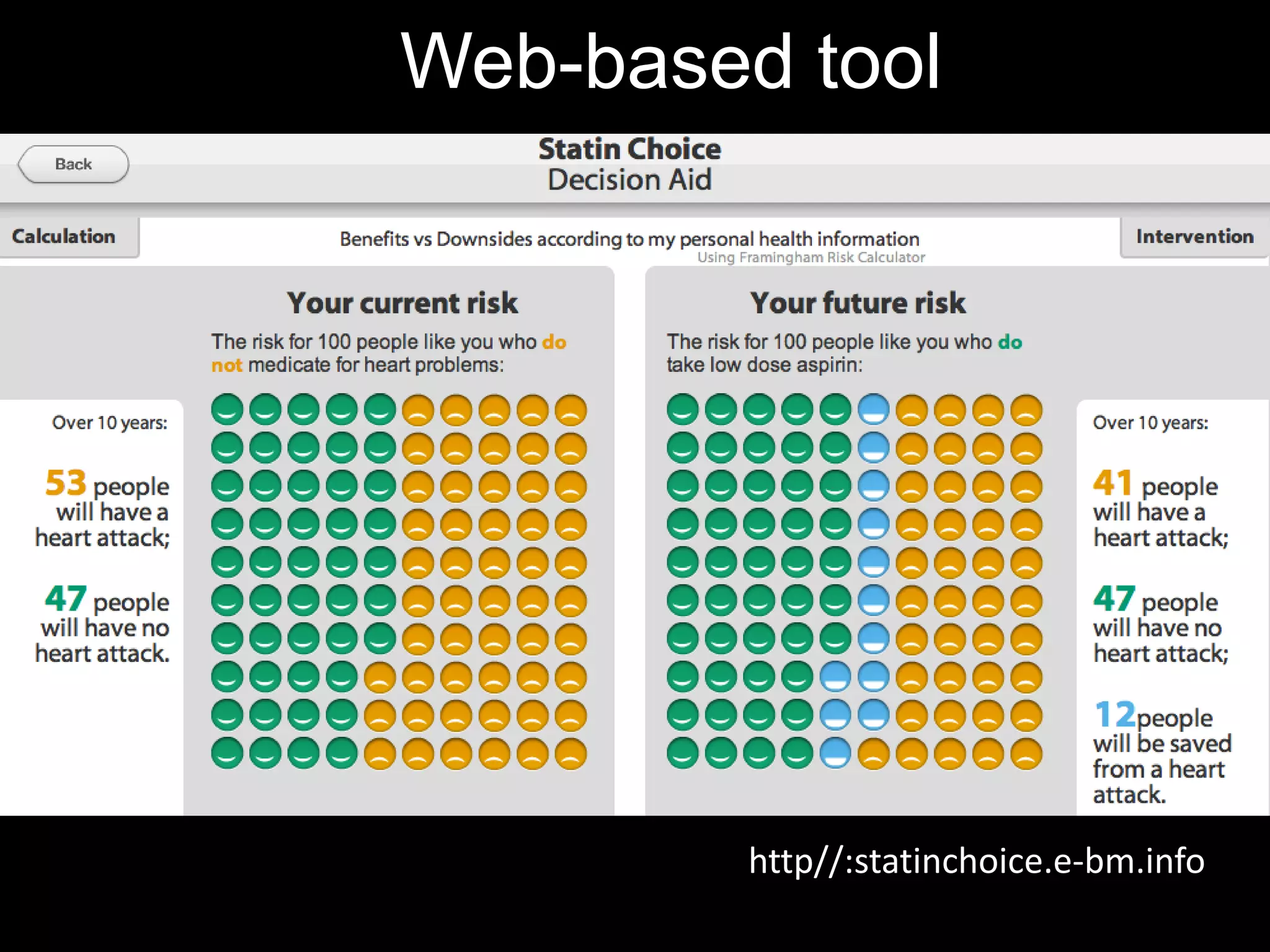
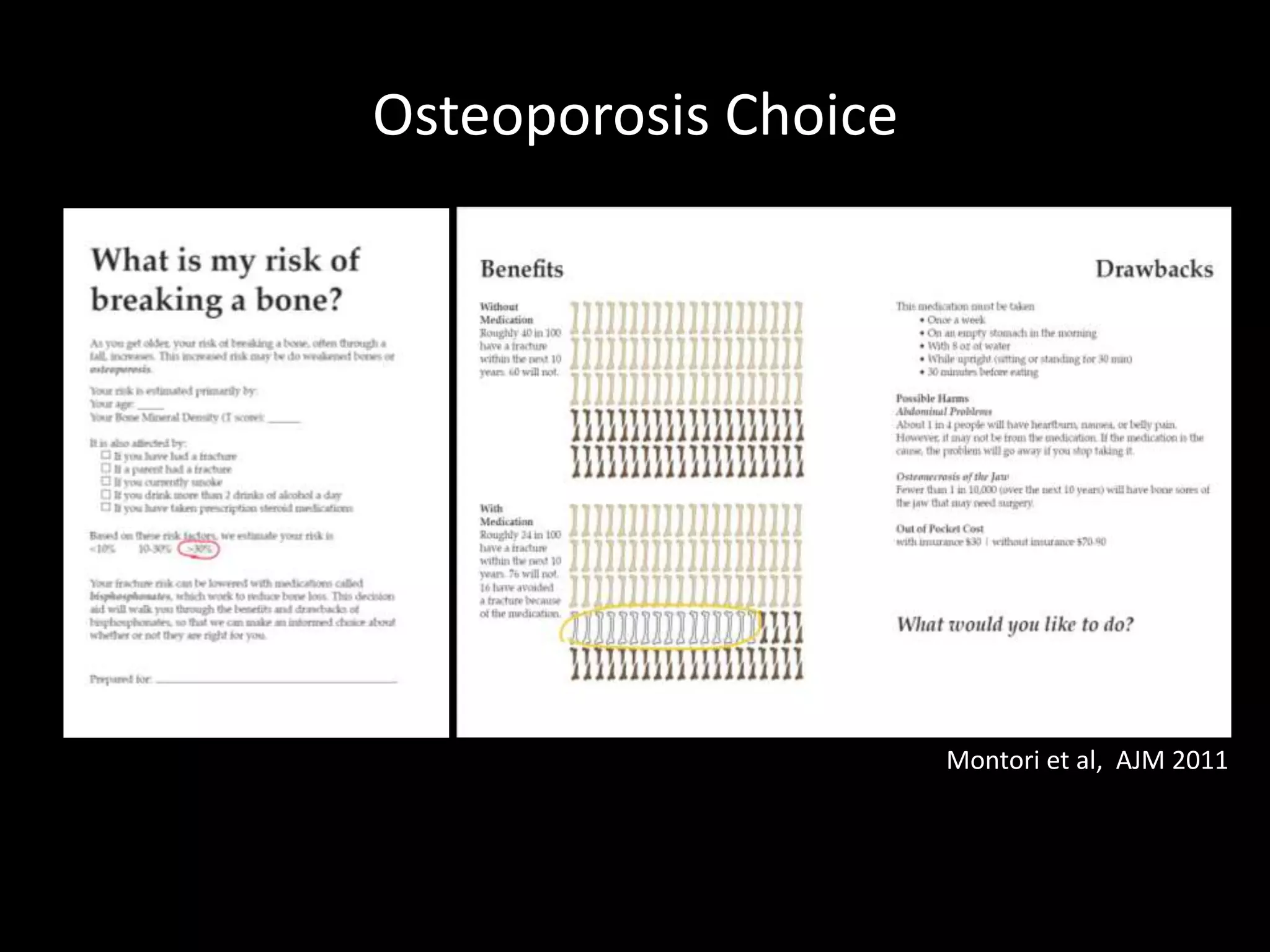
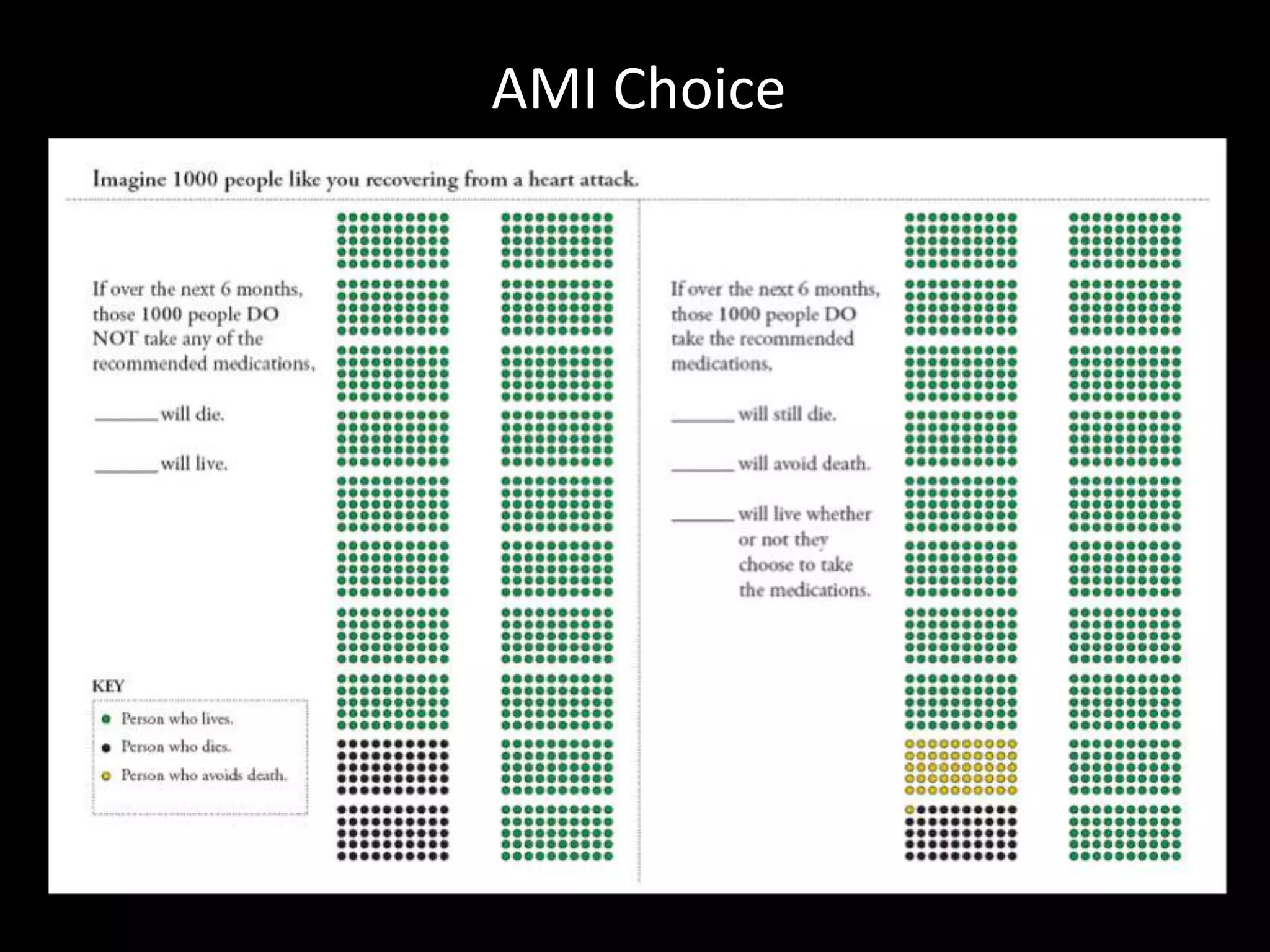
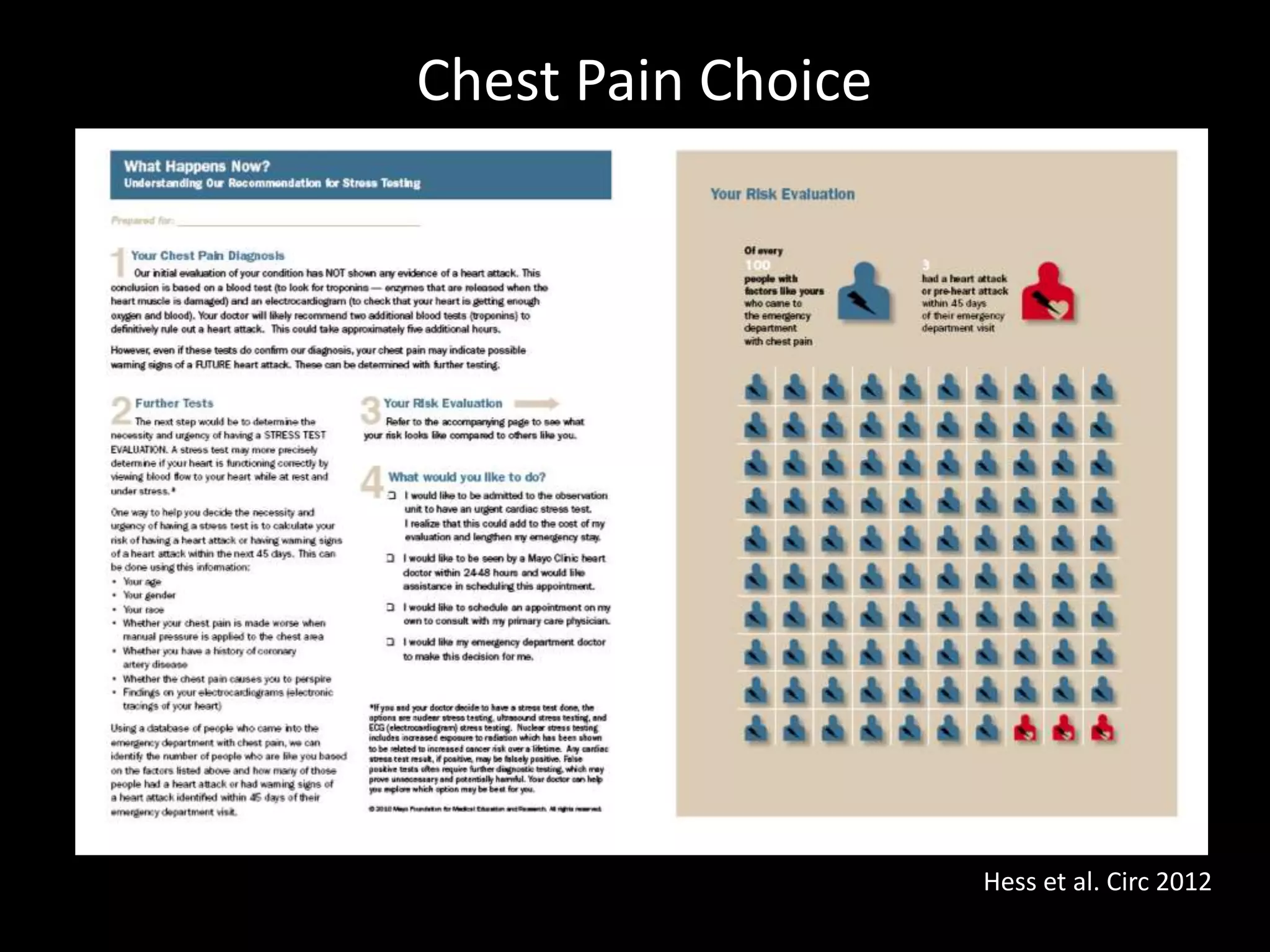
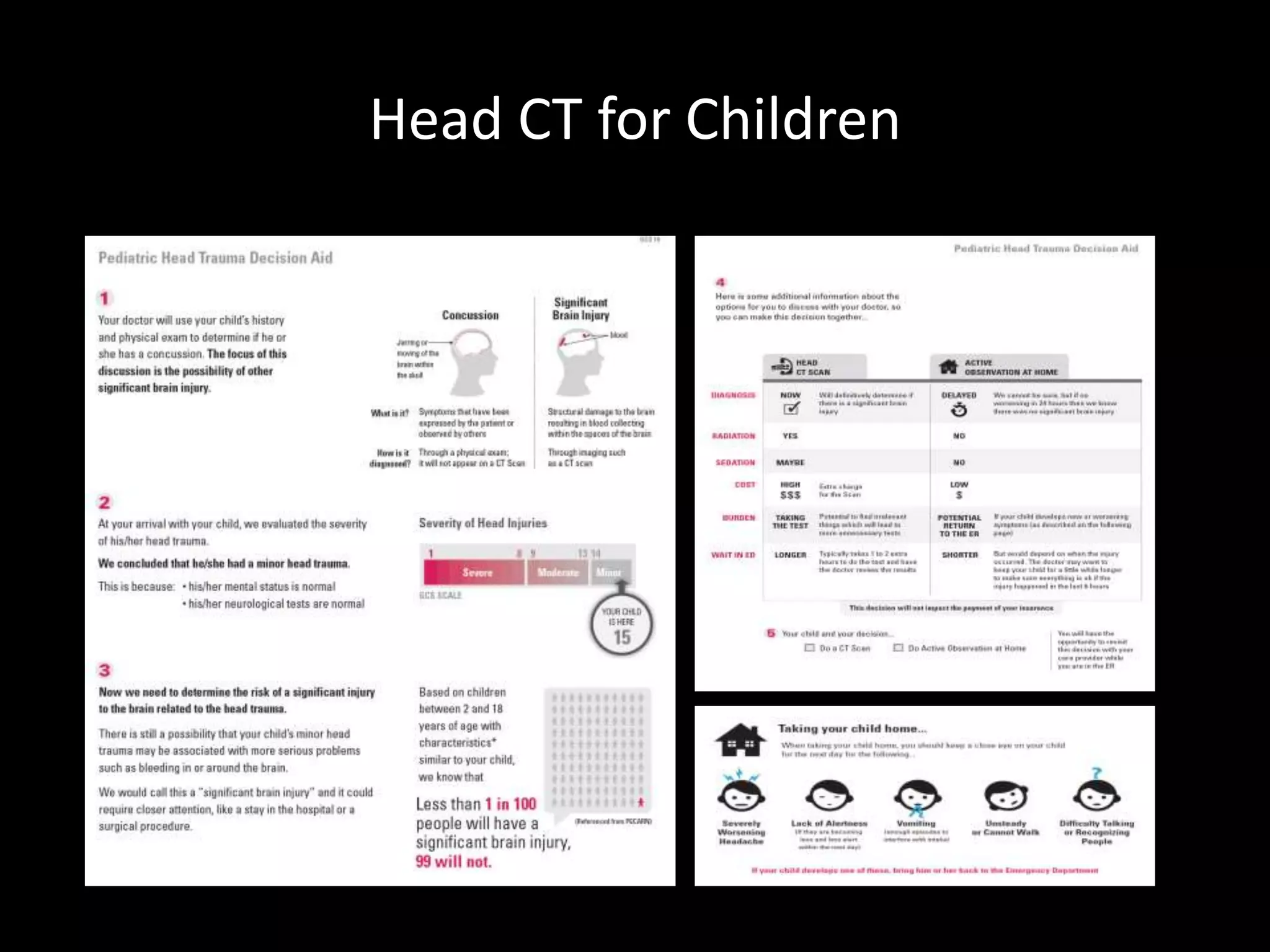
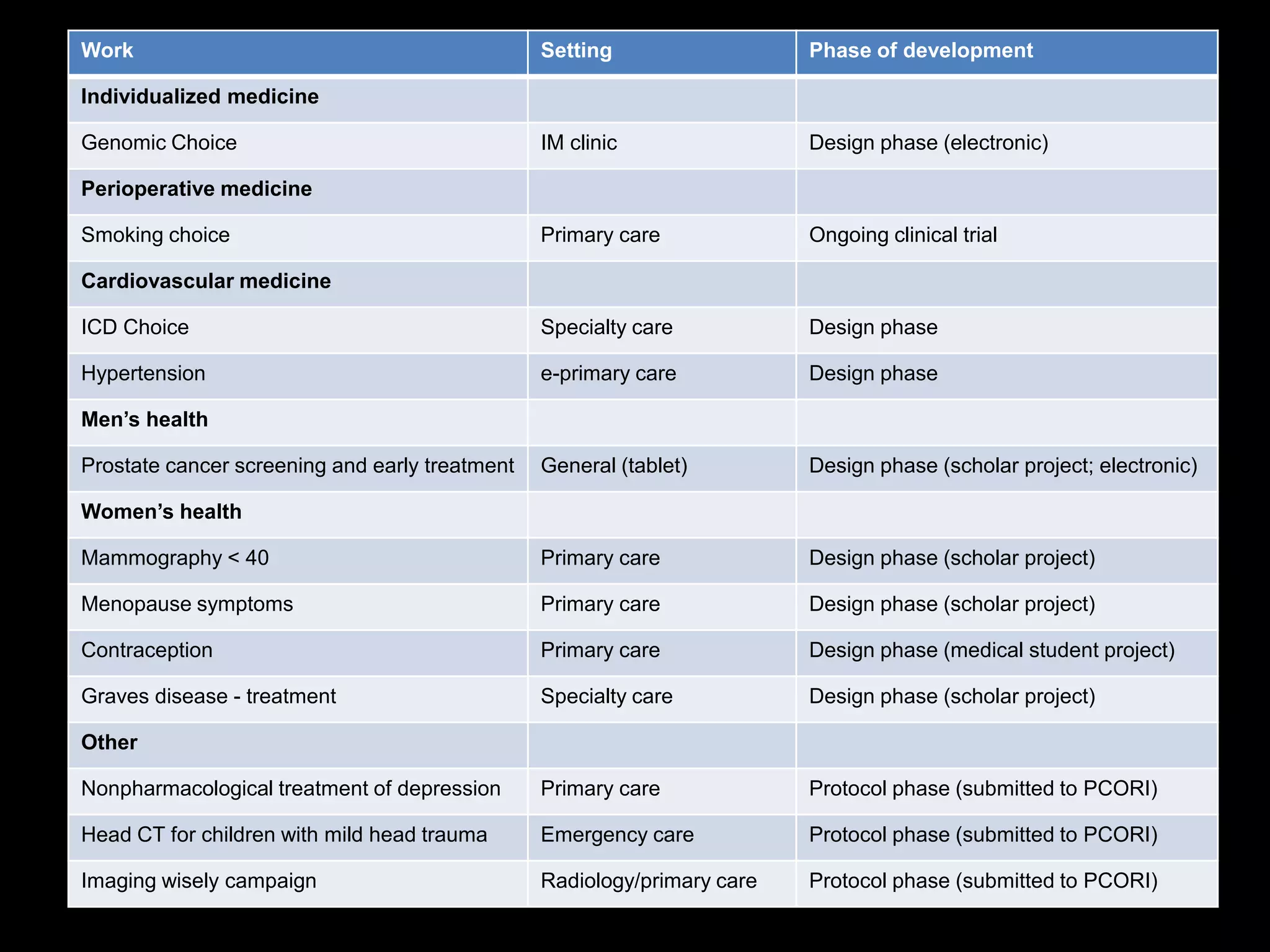
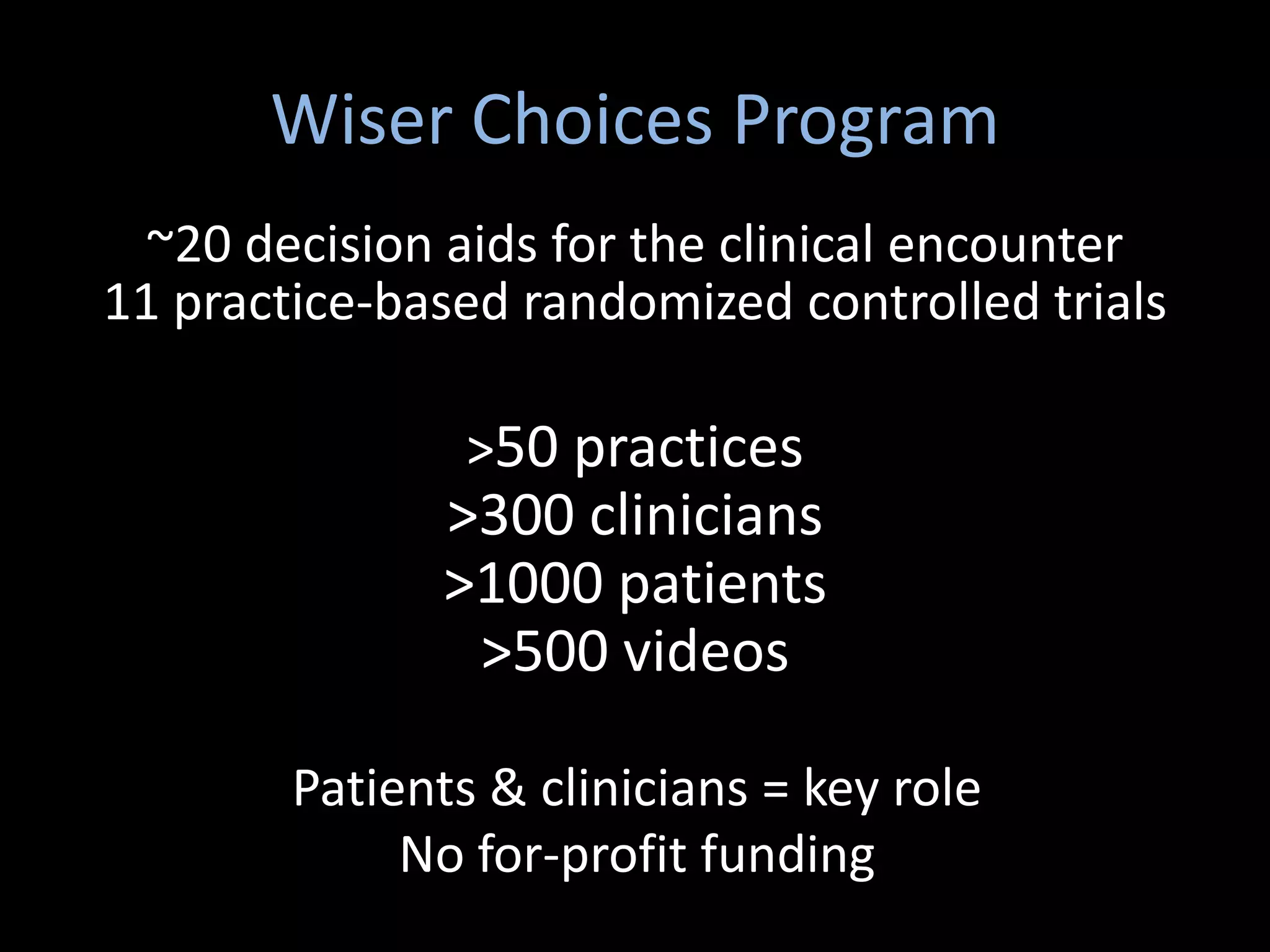
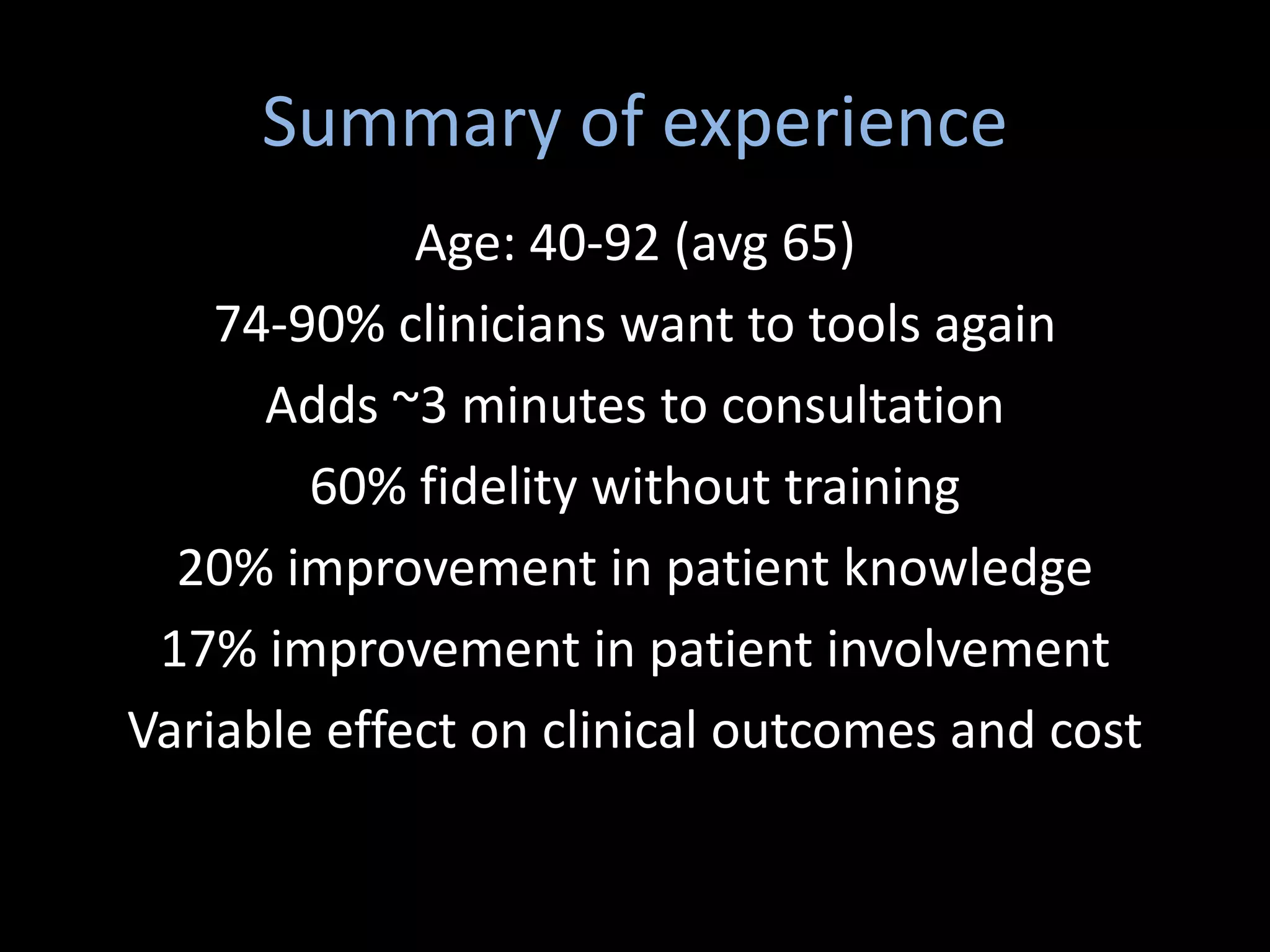
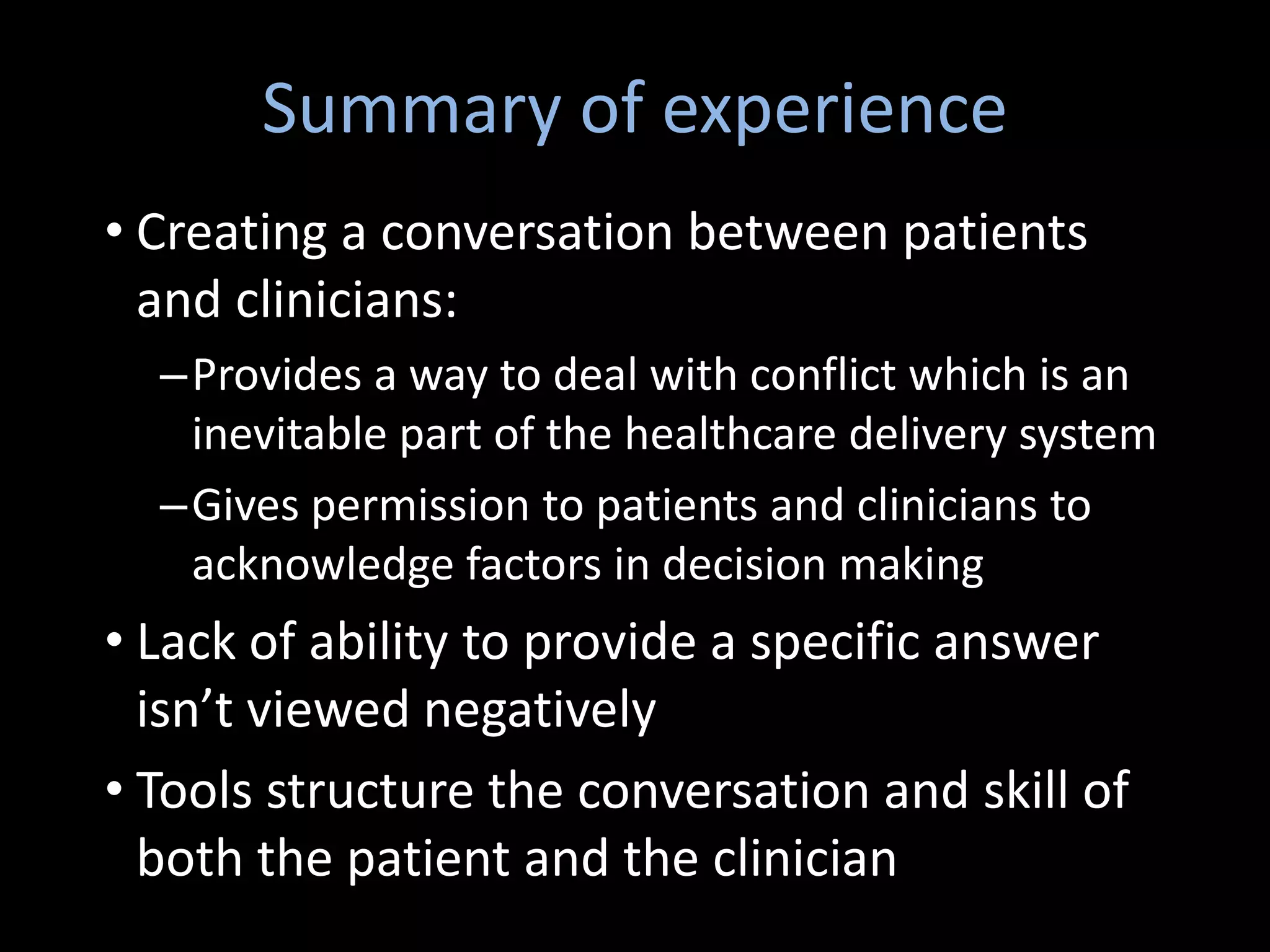
The document discusses shared decision making (SDM) in clinical encounters at Mayo Clinic. It describes the work of the Knowledge and Evaluation Research (KER) Unit, which designs and evaluates decision aids to facilitate SDM between clinicians and patients. Decision aids provide unbiased information on healthcare options and help patients consider what matters most to them. Studies show decision aids improve patient knowledge and involvement without increasing consultation time. The KER Unit has created over 20 decision aids covering various medical topics. Their goal is to create meaningful conversations centered around patient needs and values to improve healthcare outcomes and experience.