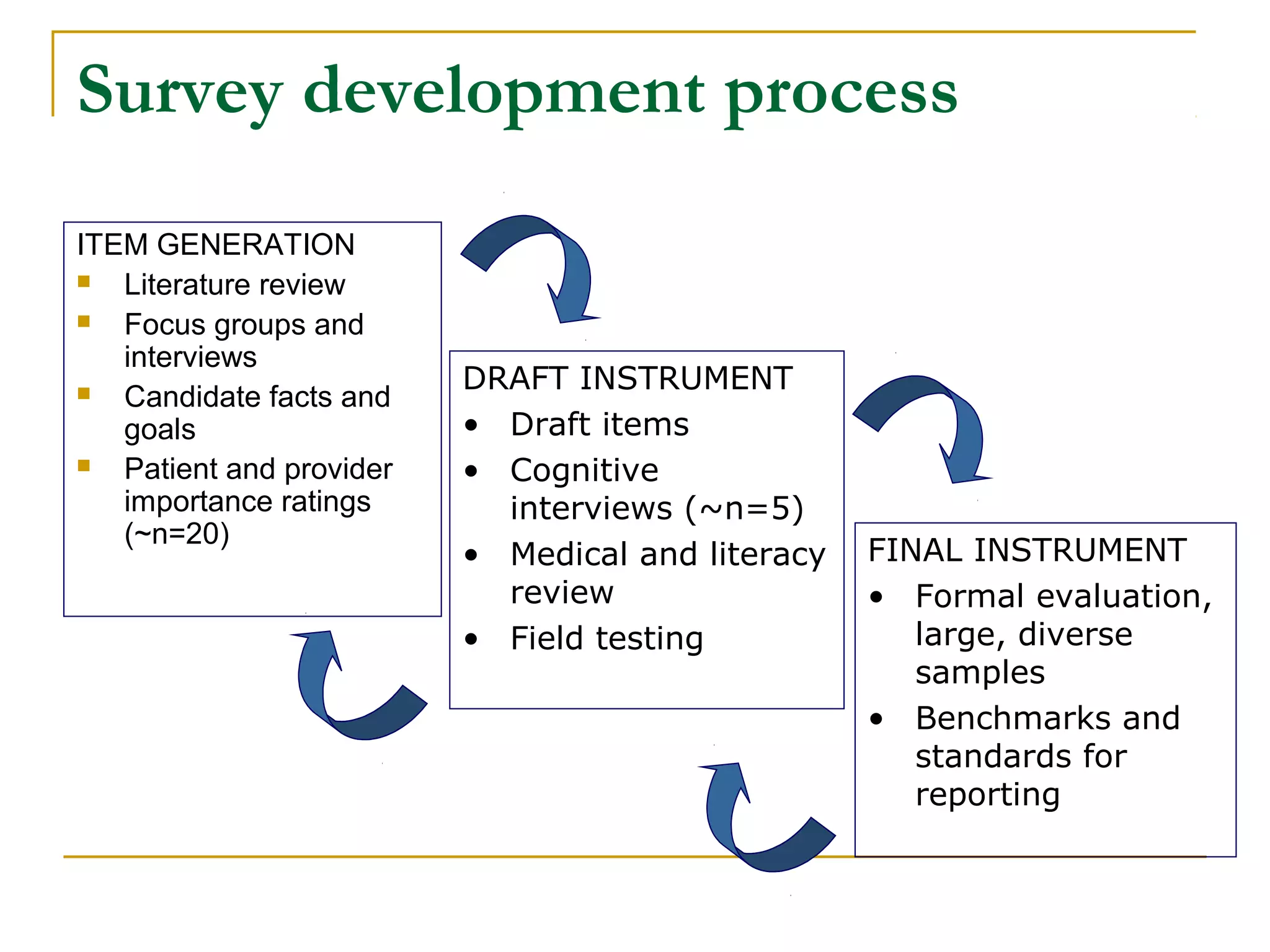
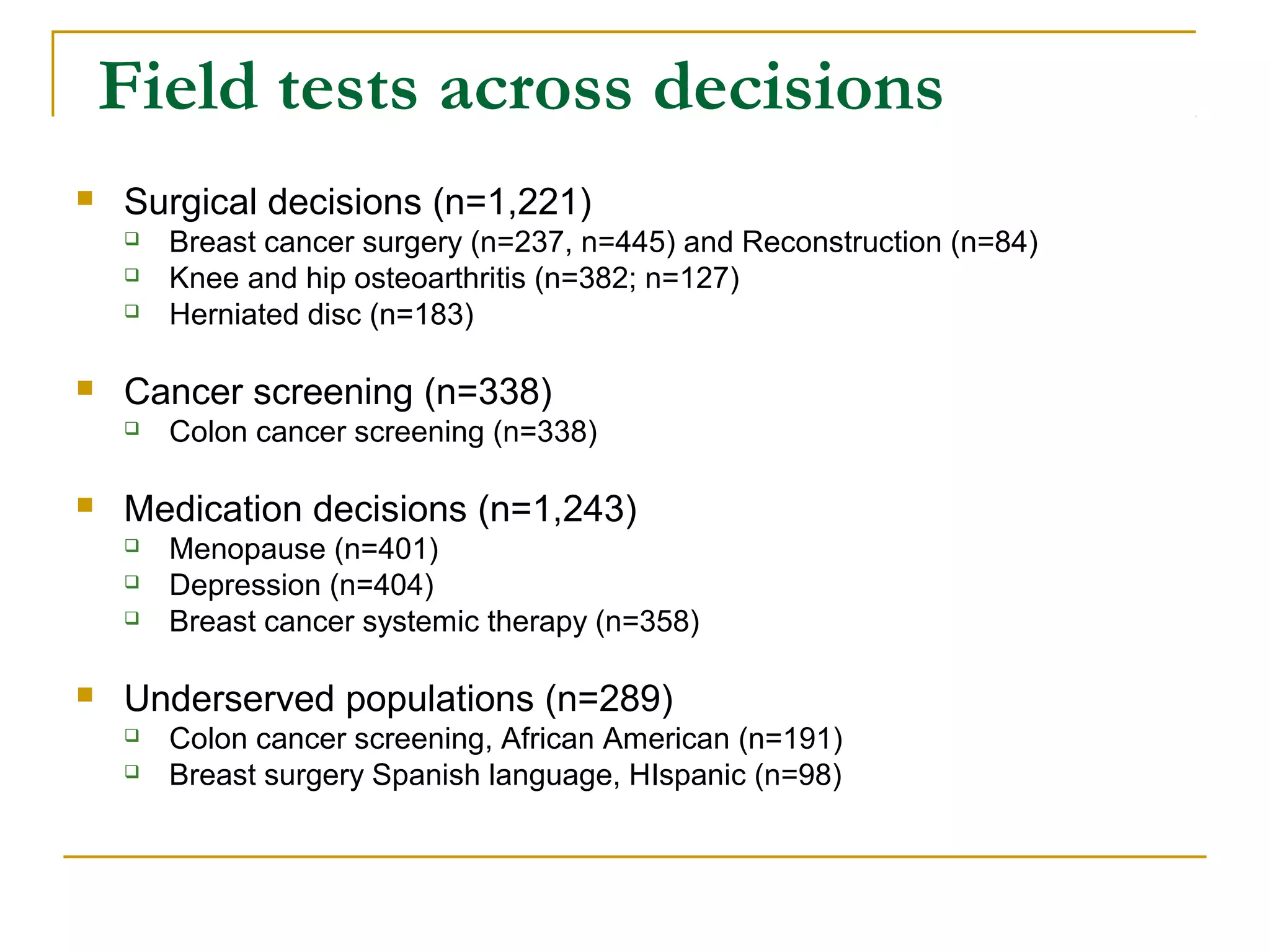
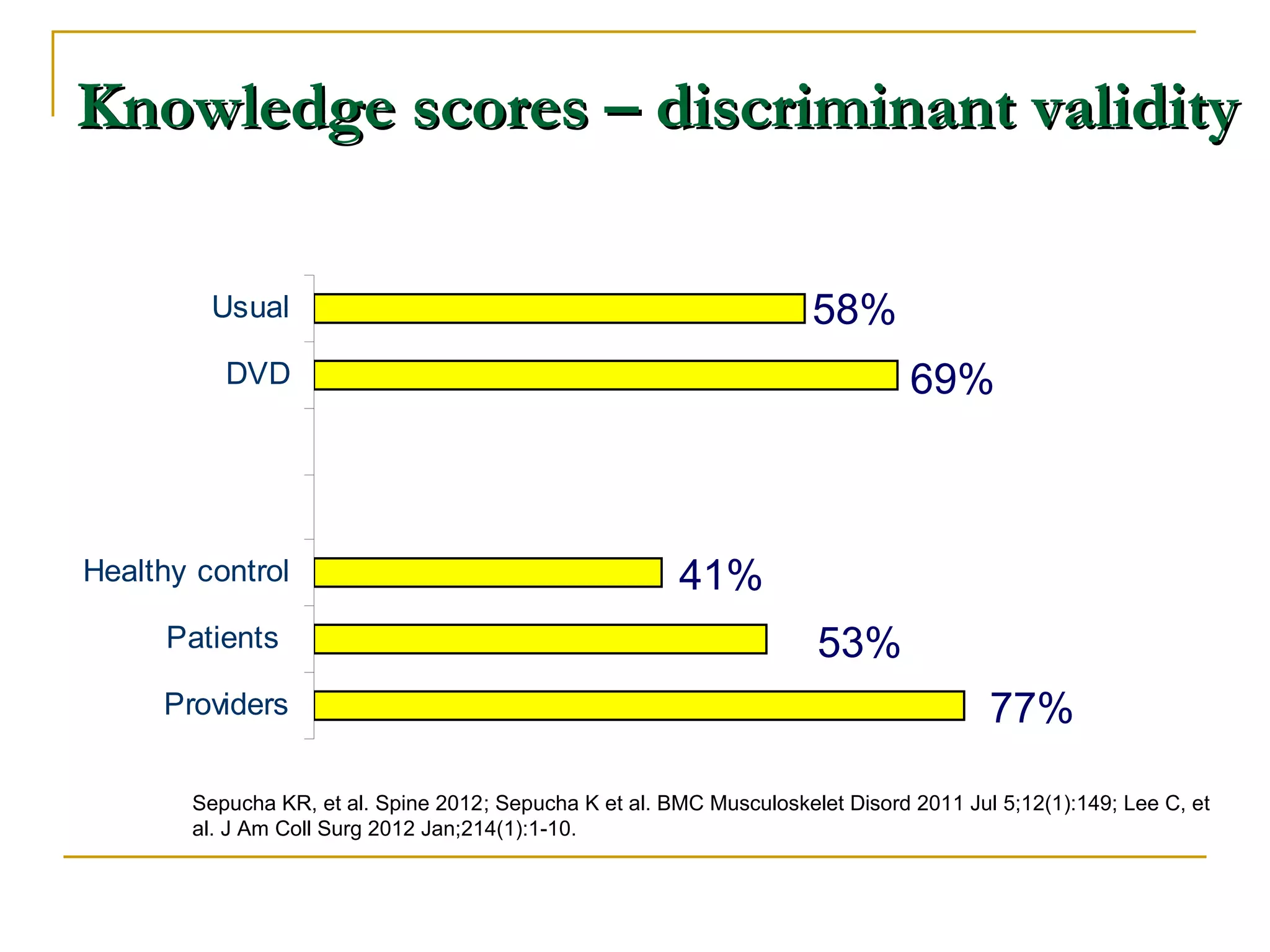
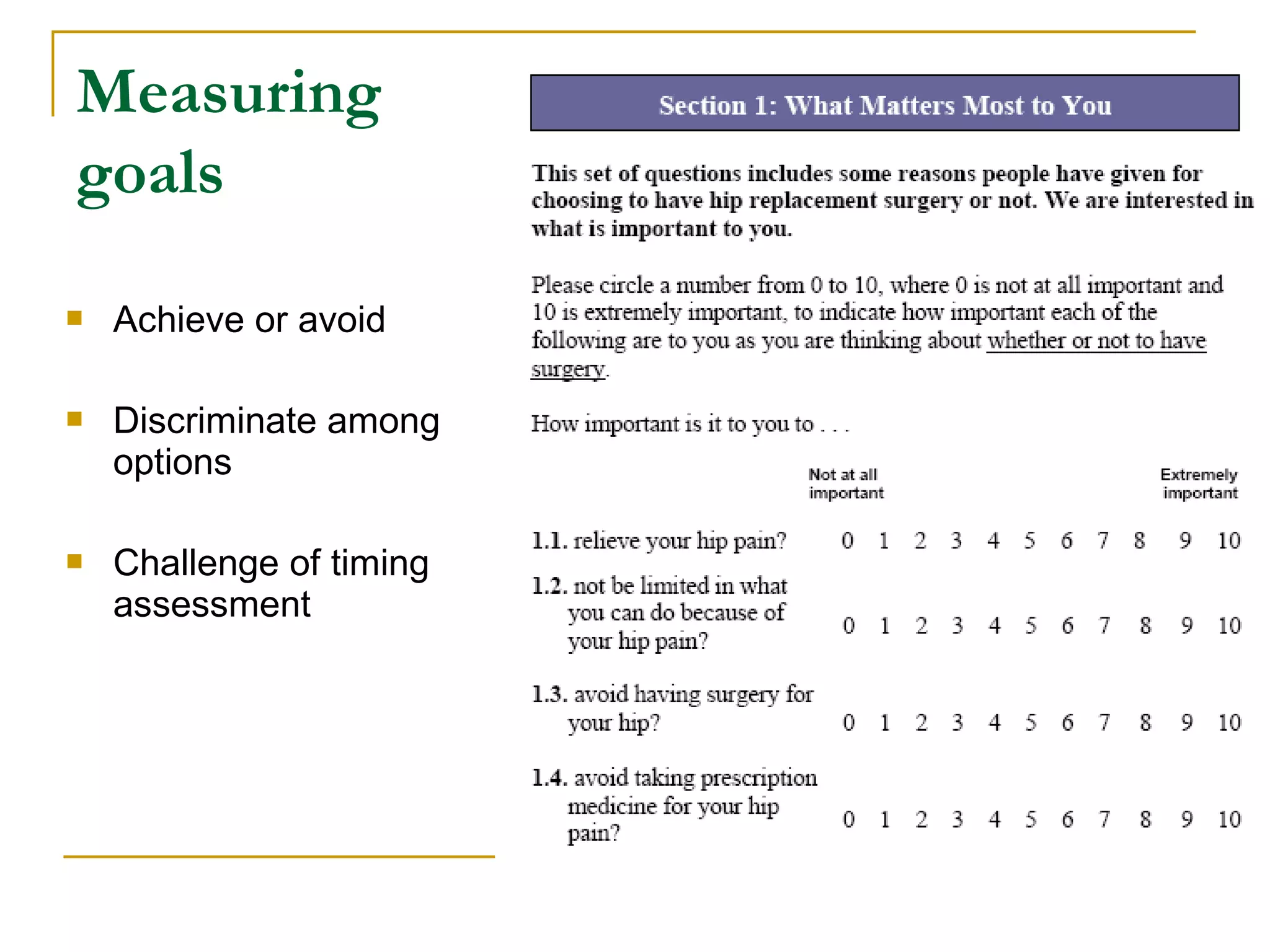
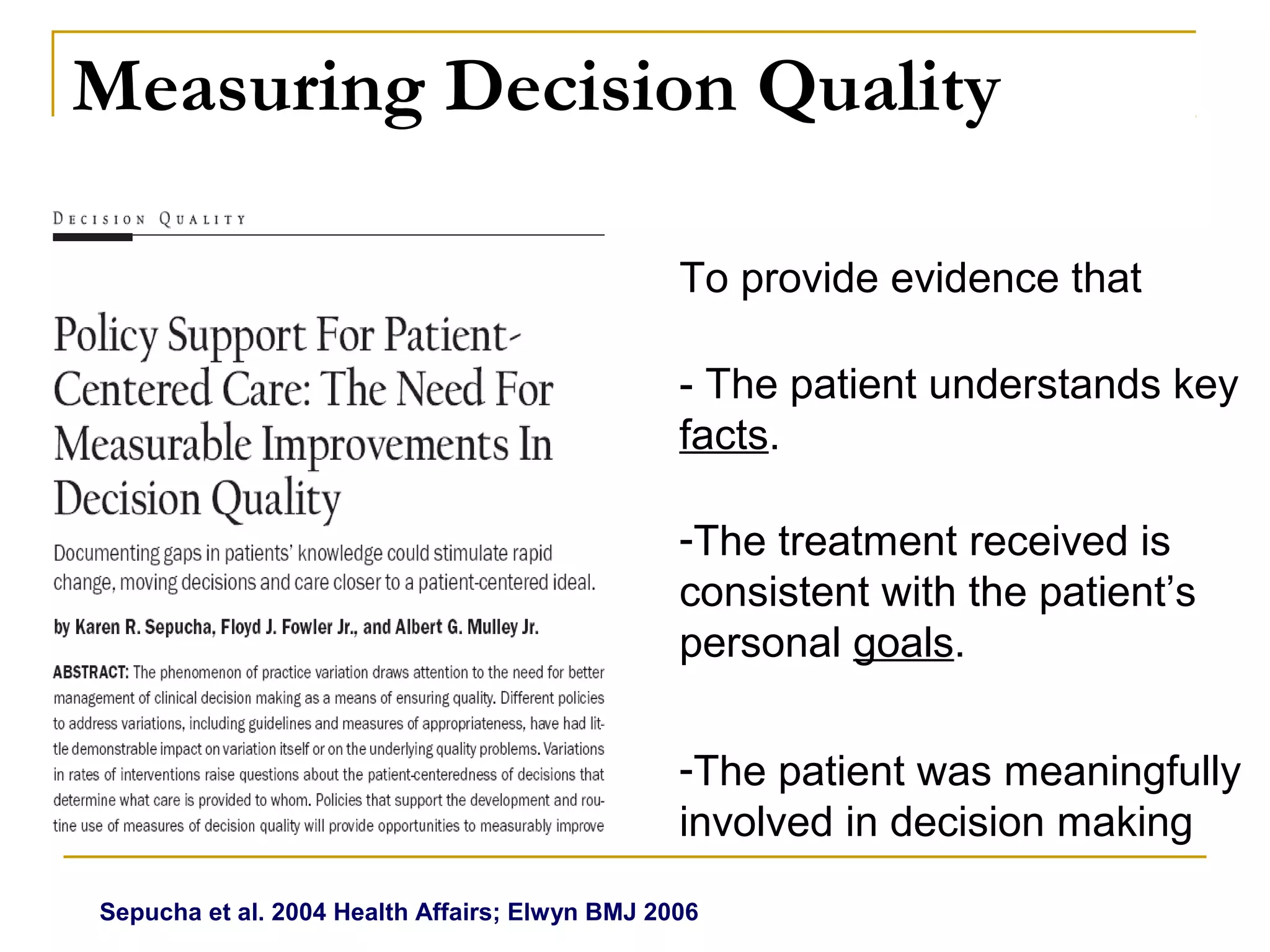
The document discusses measuring and improving decision quality in healthcare, focusing on how well patients understand treatment options and whether these options align with their personal goals. It presents a case study of a patient and outlines the importance of informed, patient-centered care, including the development and validation of survey instruments to assess decision quality. The ultimate goal is to enhance research, clinical practice, and accountability by ensuring patients are knowledgeable and involved in their treatment decisions.
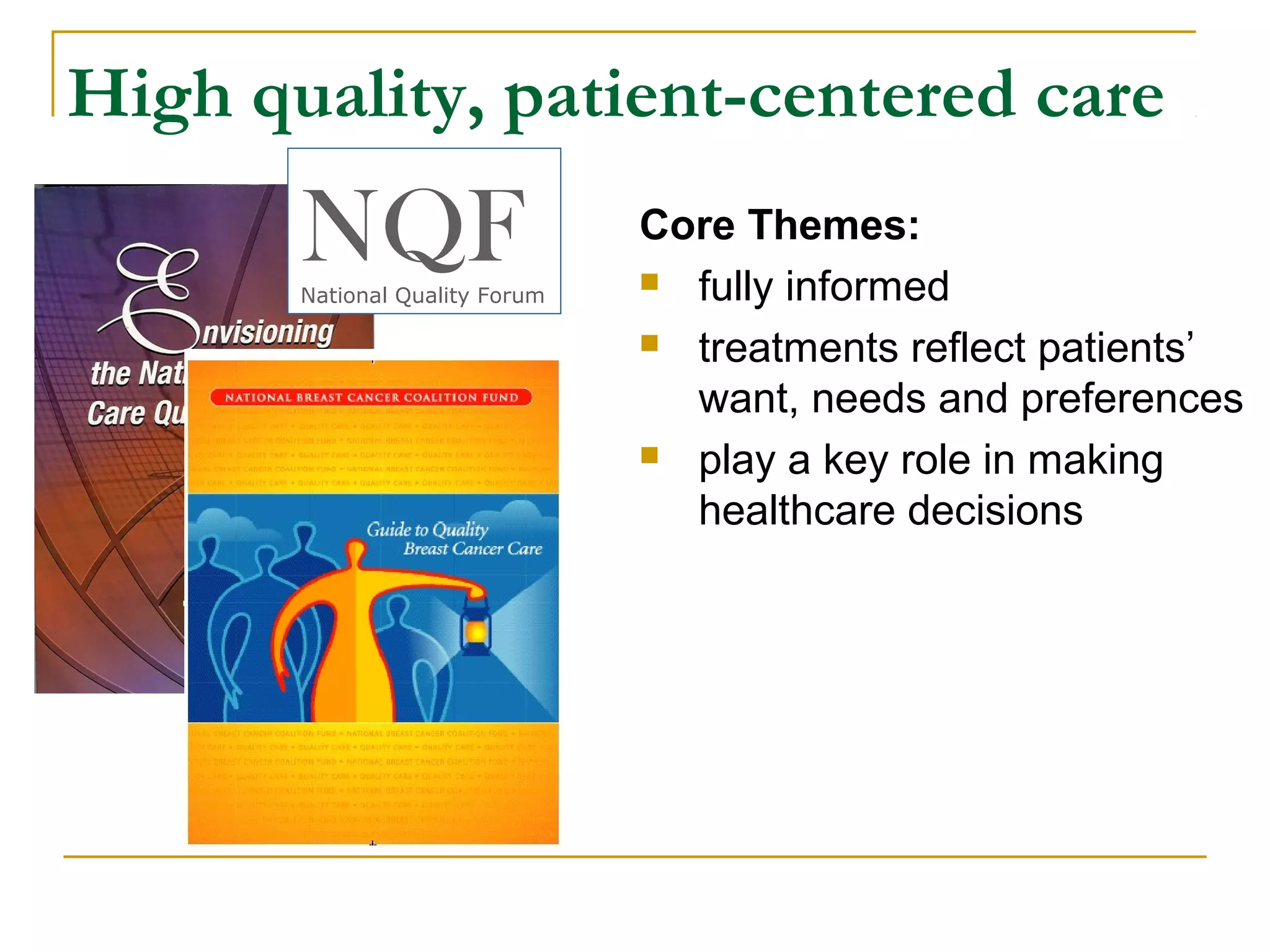
![Who made the decision about treatment of
your breast cancer?
“they didn’t say to me, “Well, we could
remove the breast, we could do this,
we could do that.” They just said, “This
is what we’re going to do.” And that
Mainly the doctor
was it—I wasn’t in on the decision.”
“She was compassionate, … [and] gave
me the data that I needed ... We talked
statistics and sizes and measurements
X Both equally
and things that helped me..with my
decision.”
“I made the decision. I’m very happy with
the lumpectomy because that’s what I
wanted to do from the beginning. They
Mainly you [my doctors] didn’t disagree. They didn’t
agree. They just said, “Okay.” They
understood.”](https://image.slidesharecdn.com/130311sepuchadqwebinar-130322081625-phpapp02/75/Measuring-and-Improving-Decision-Quality-9-2048.jpg)