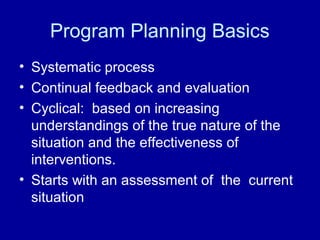
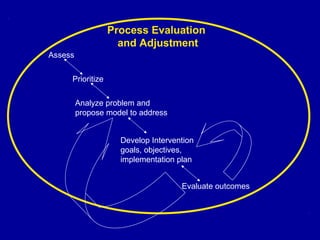
This document outlines the steps for conducting a community nutrition assessment to inform program planning. It discusses:
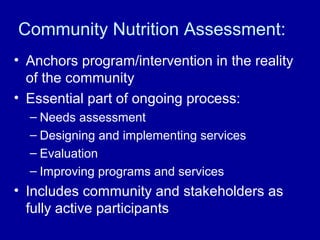
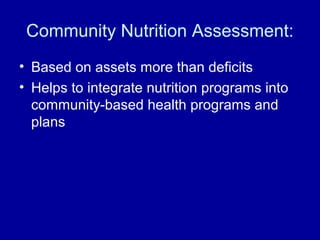
- The importance of assessment in anchoring programs in community reality and engaging stakeholders.
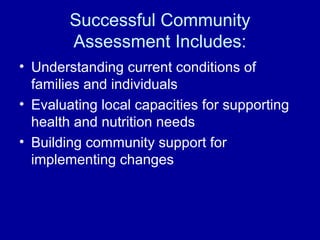
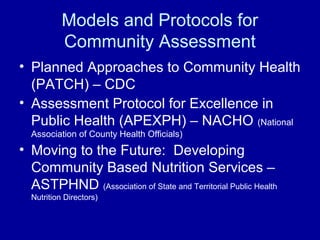
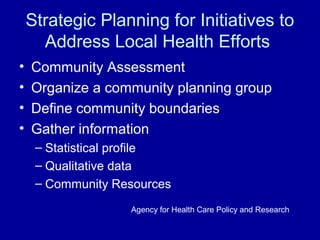
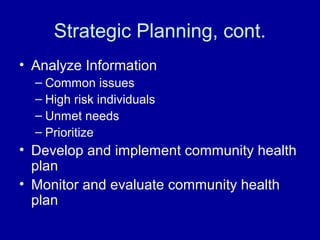
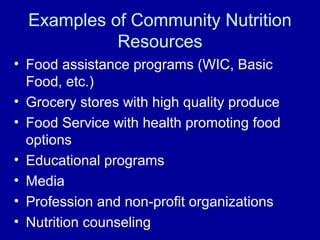
- Models for assessment including understanding community conditions, capacities, and identifying priority issues.
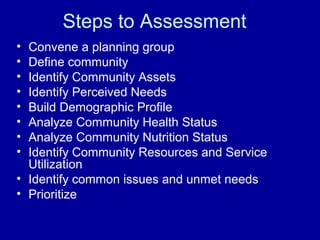
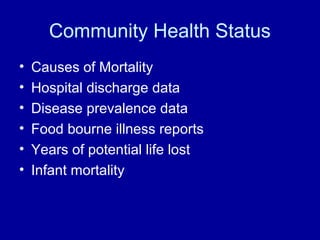
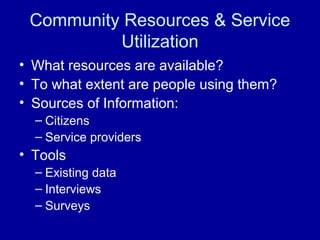
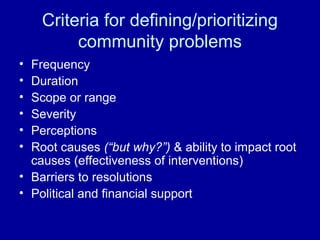
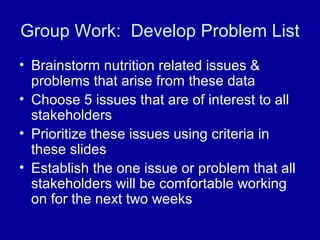
- Key steps like convening a planning group, collecting demographic and health status data, identifying resources and prioritizing issues.
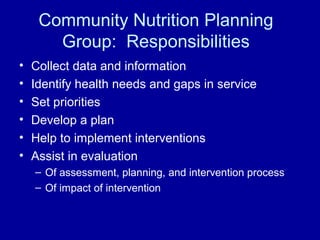
- The role of the planning group in gathering data, setting priorities, developing and evaluating plans and interventions.