The document summarizes three family planning projects implemented by the Uganda Protestant Medical Bureau (UPMB) and the involvement of religious leaders. It discusses:
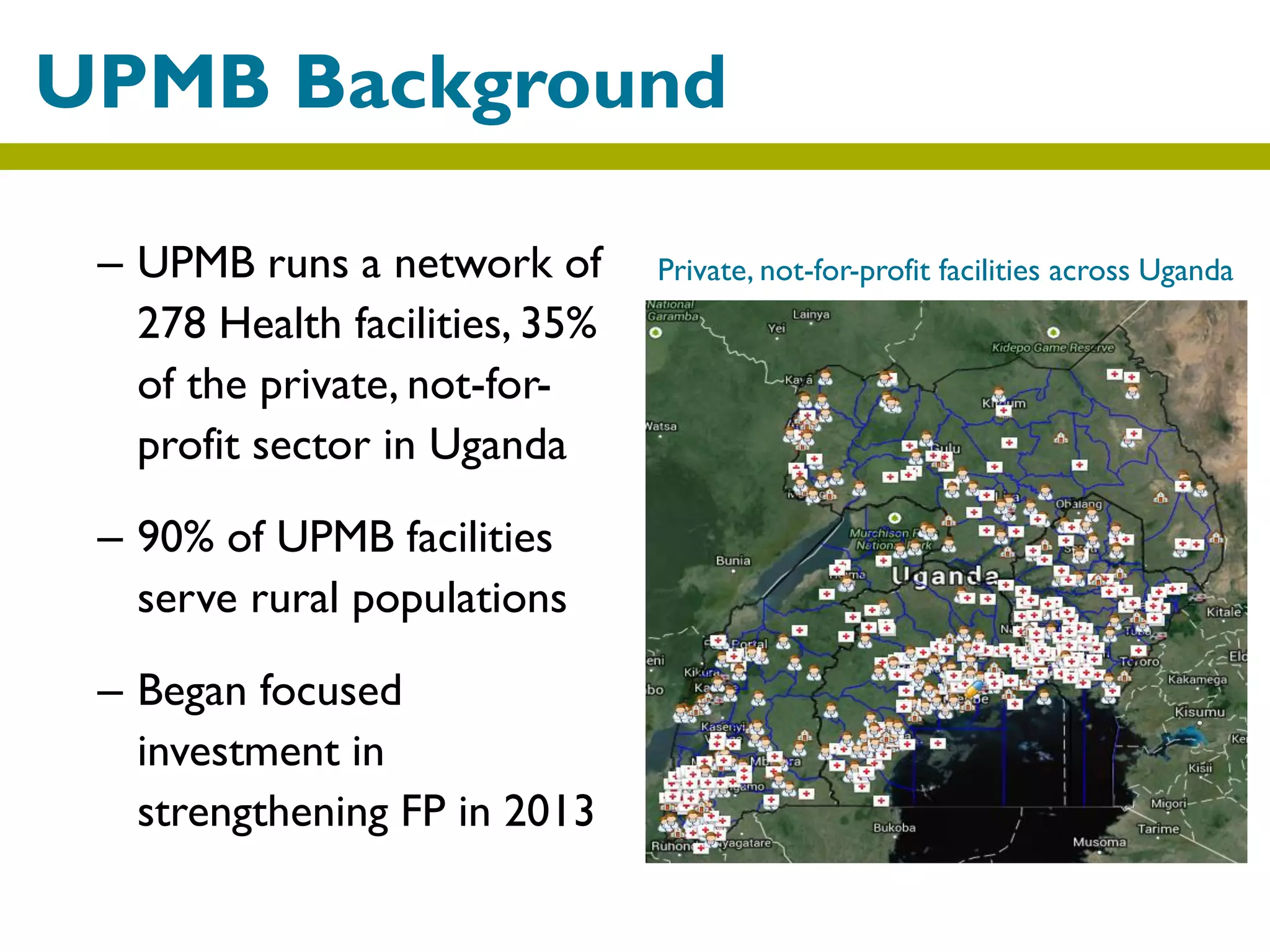
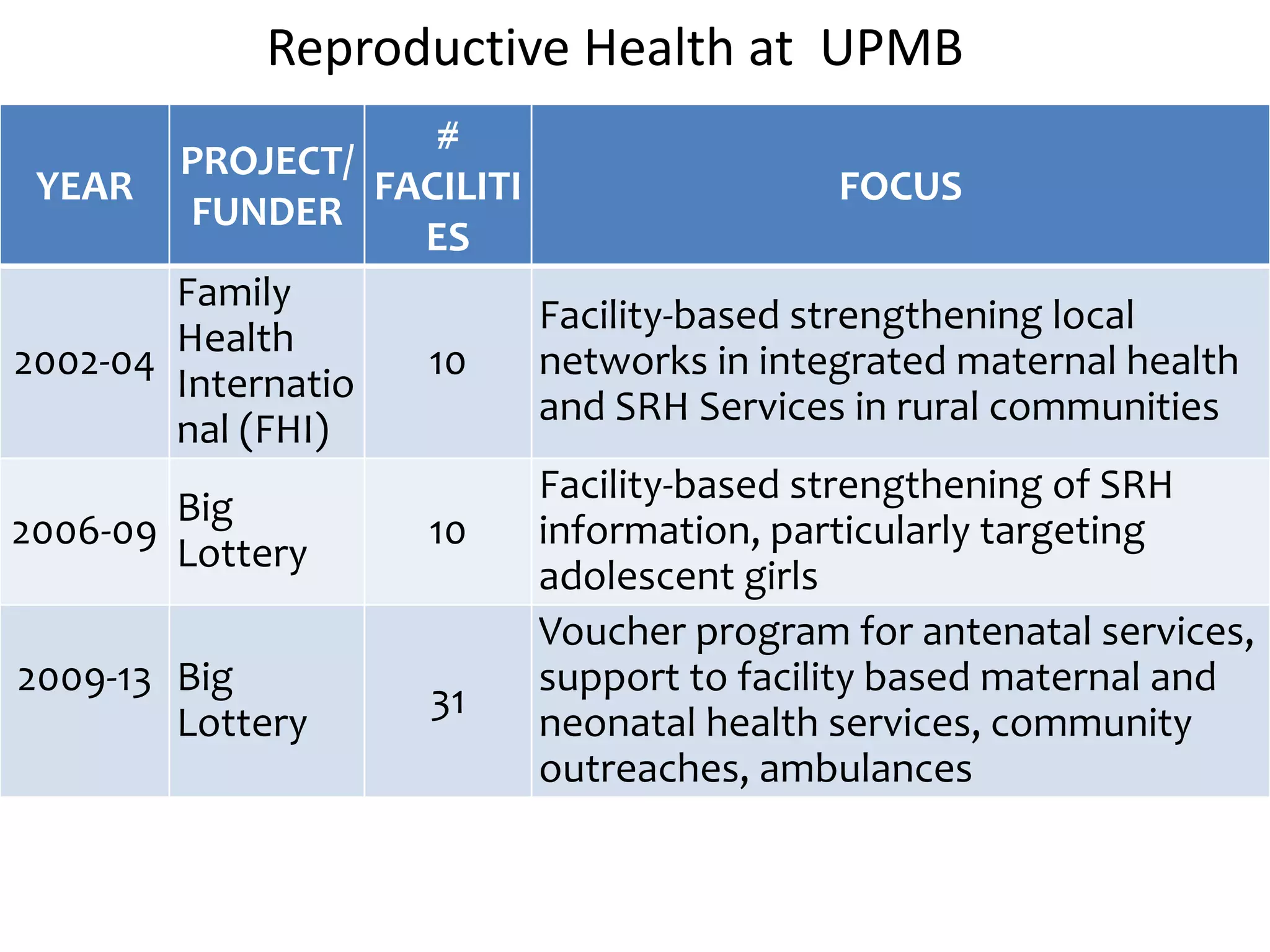
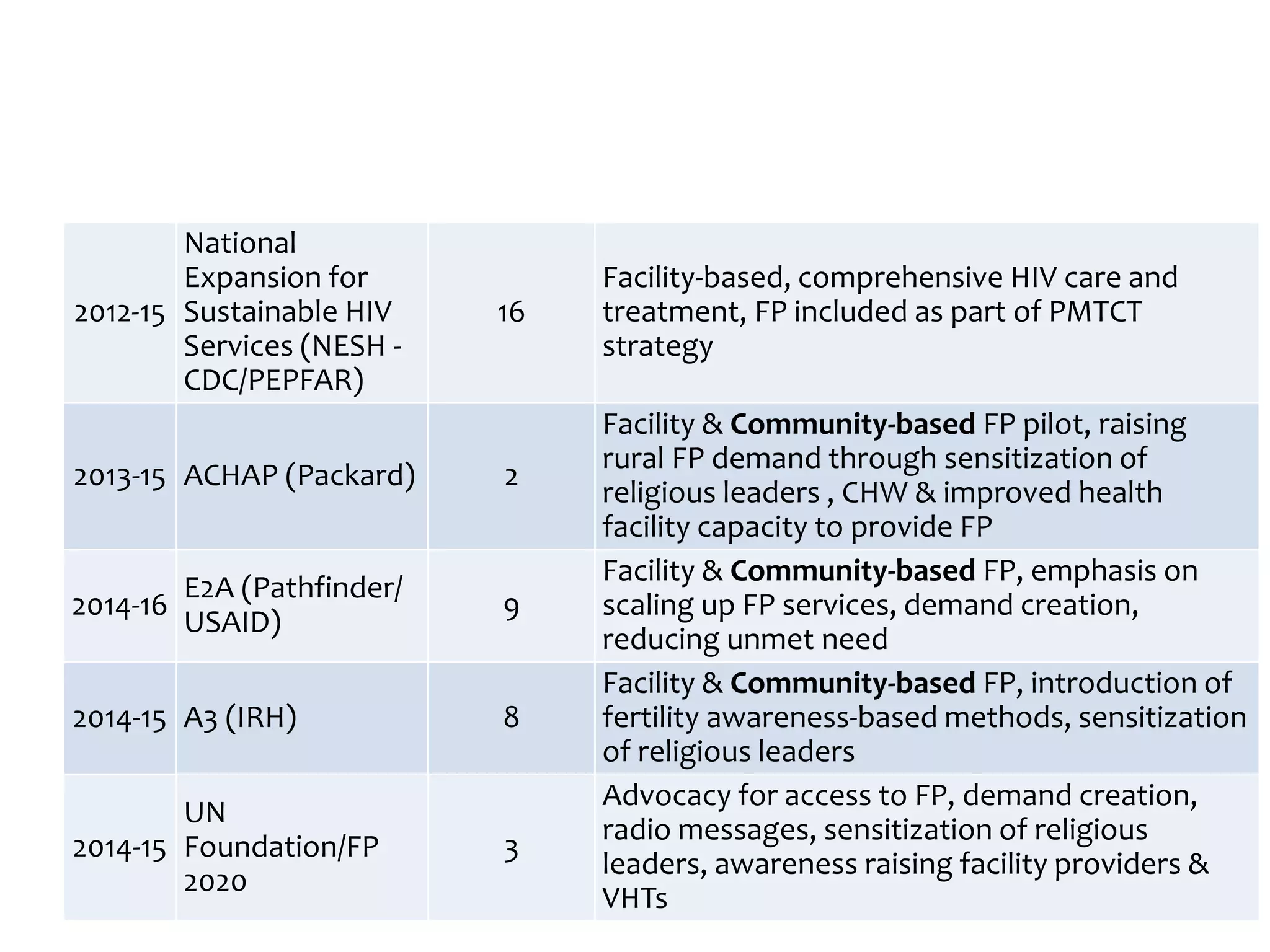
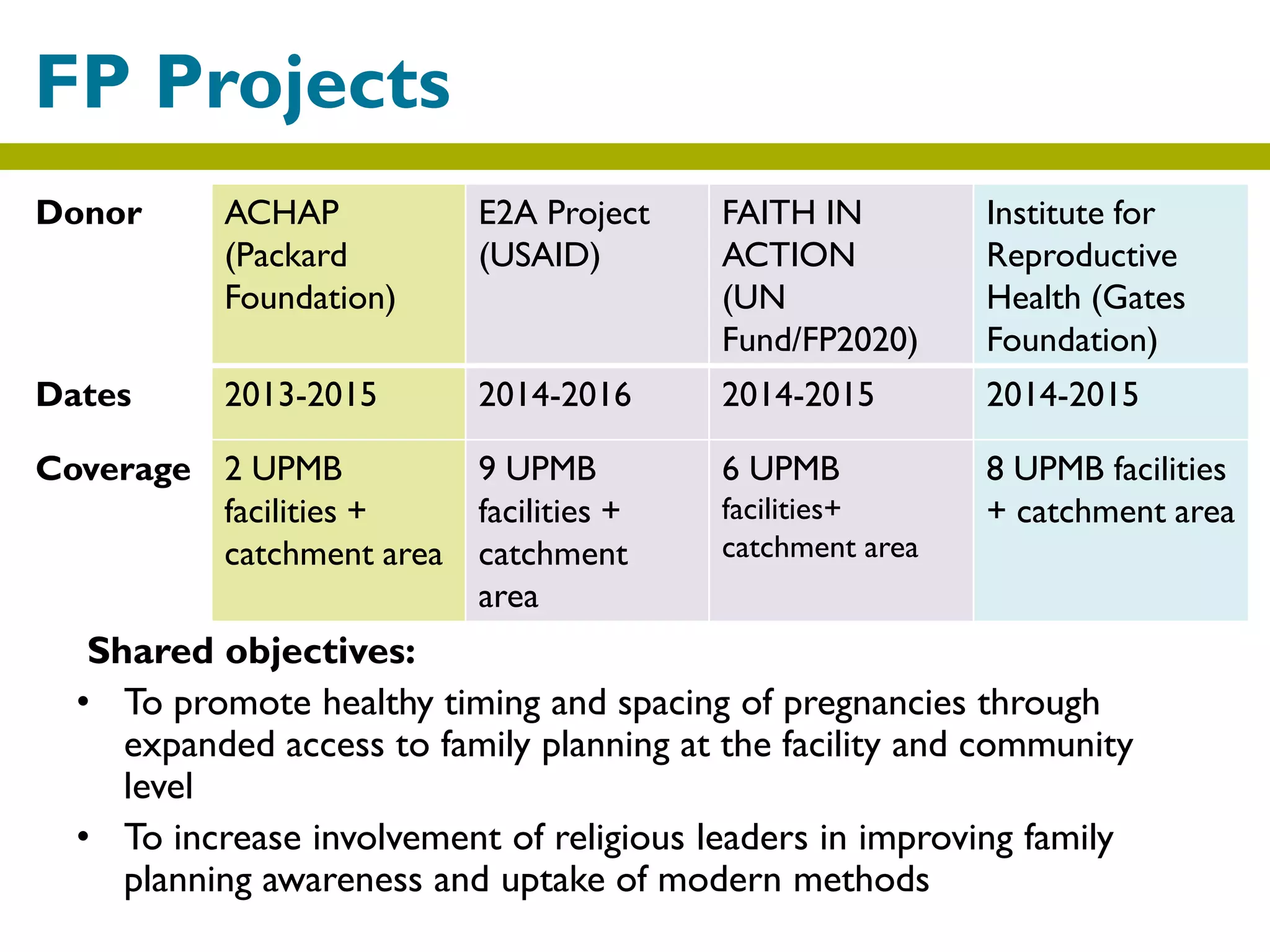
1) UPMB runs a network of 278 health facilities, serving mostly rural populations, and began focusing on strengthening family planning in 2013.
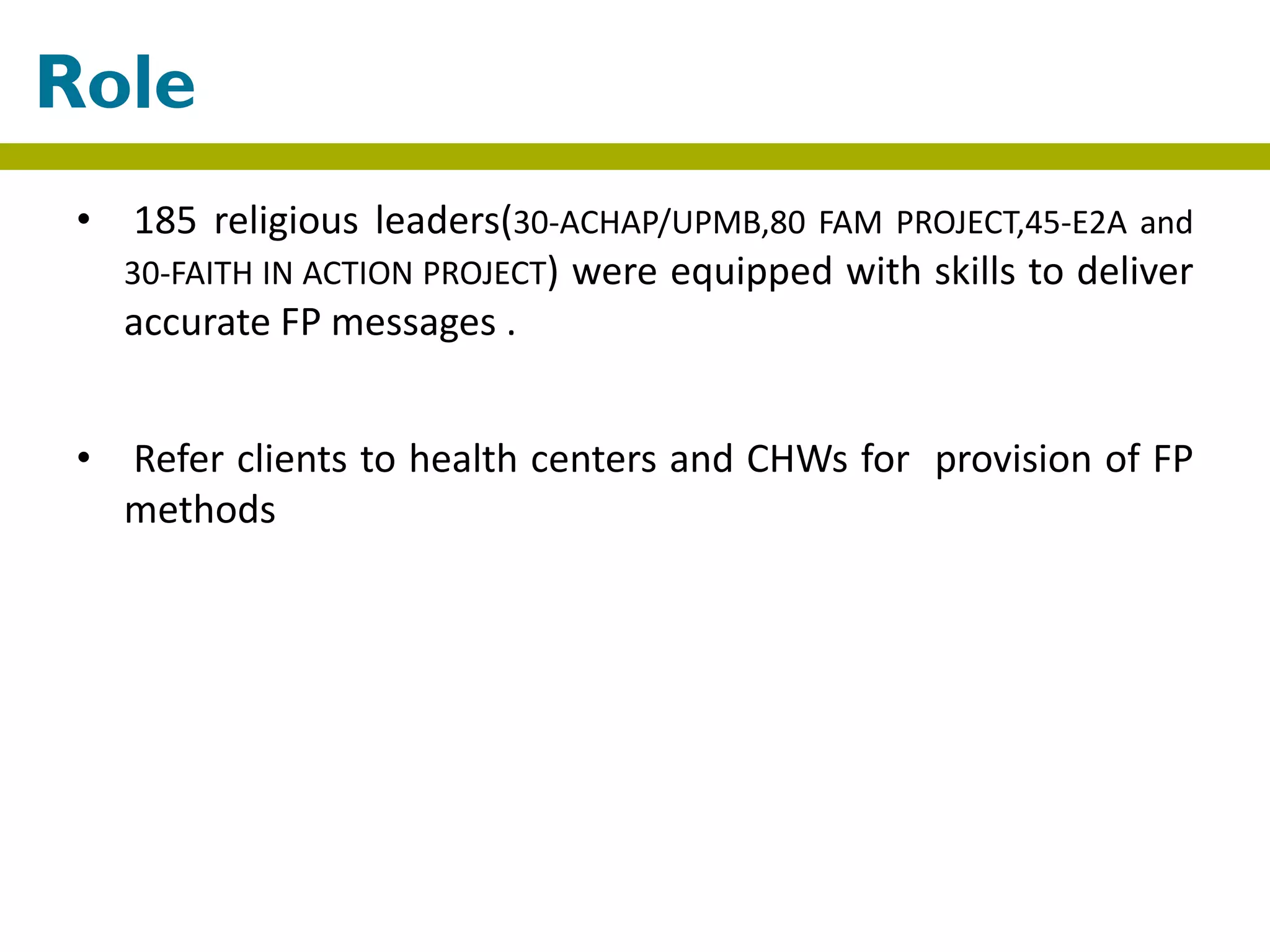
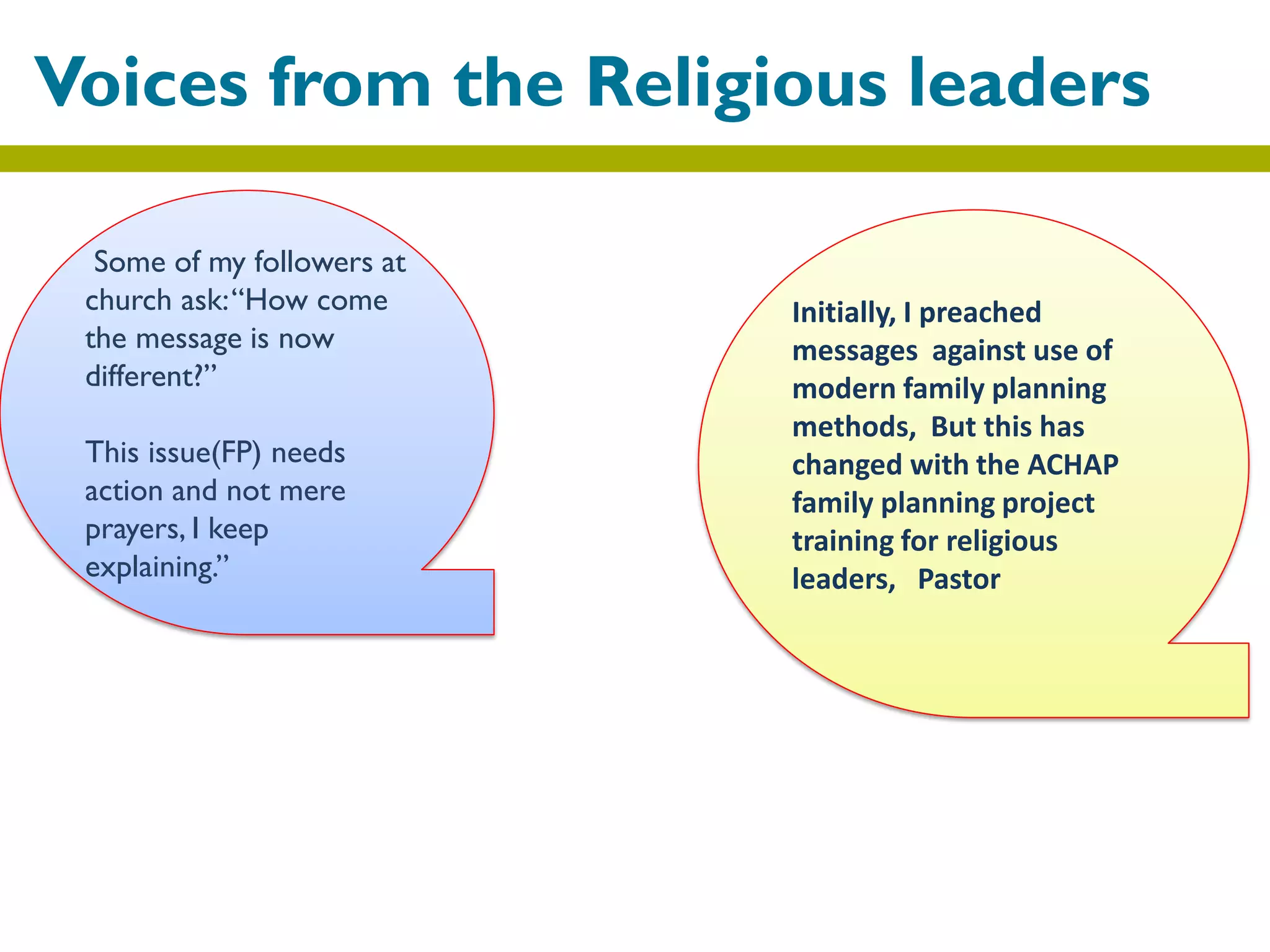
2) The projects trained 185 religious leaders to deliver accurate family planning messages and refer clients to health centers, increasing facility referrals three-fold.
3) Religious leaders now act as ambassadors by educating communities and creating platforms for health workers, changing attitudes towards family planning.