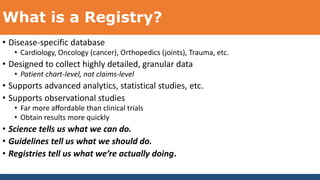
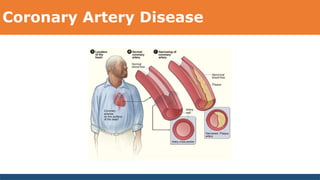
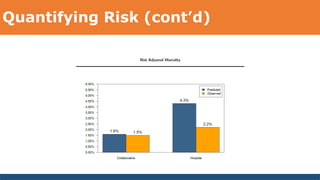
The document discusses the role of clinical healthcare data analytics, particularly within interventional cardiology, emphasizing the importance of registries for improving patient care quality while reducing costs. It highlights healthcare's significant challenges, including rising costs and inconsistent quality, and advocates for the use of advanced analytics and technology to address these issues. A focus is placed on data quality, the necessity for actionable clinical quality measures, and a multi-level healthcare analytics adoption model to improve healthcare outcomes.