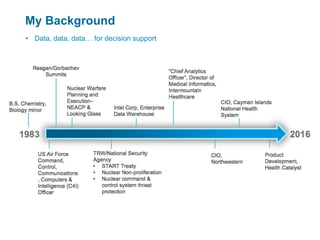
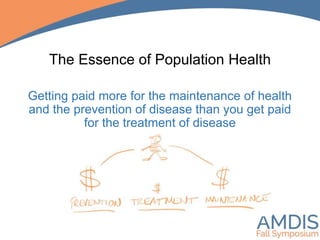
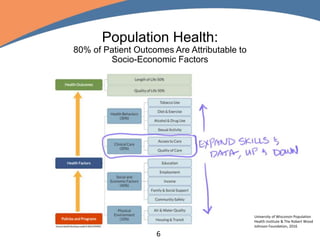
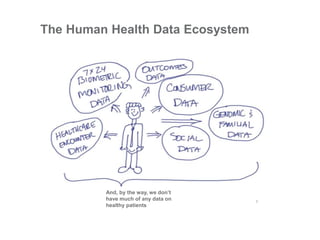
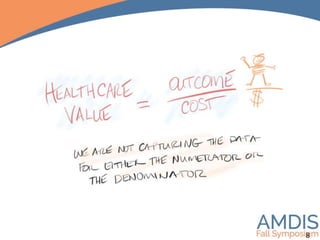
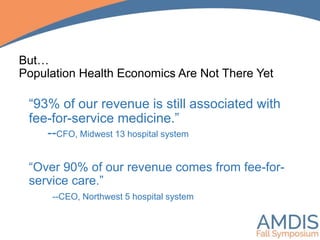
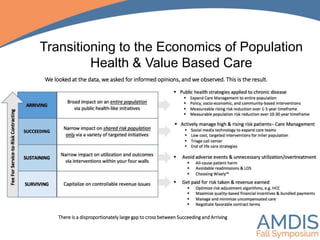
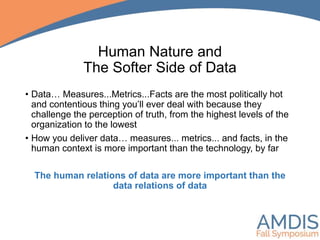
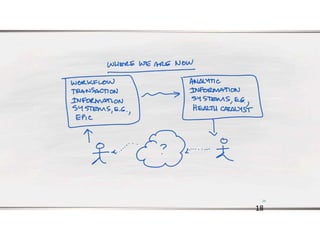
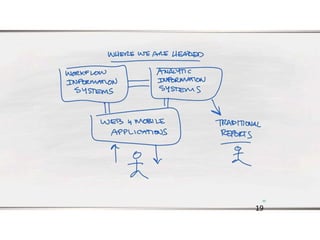
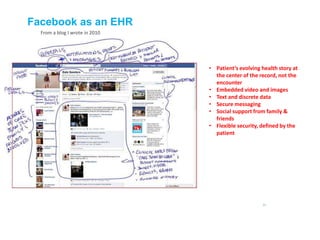
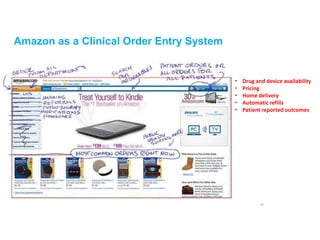
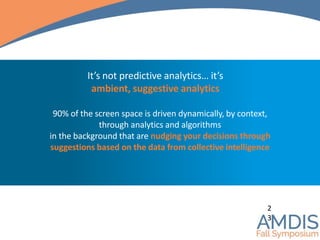
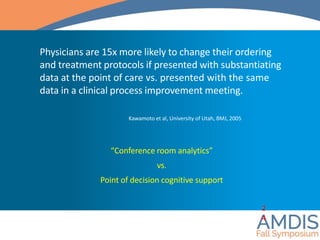
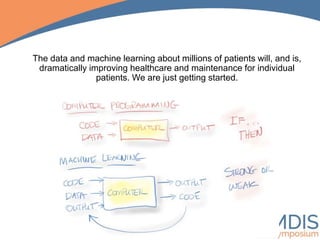
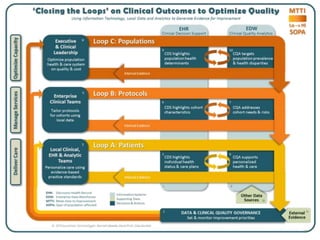
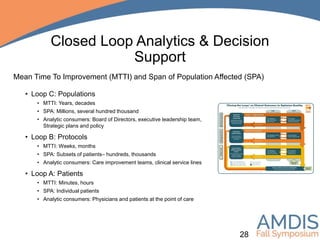
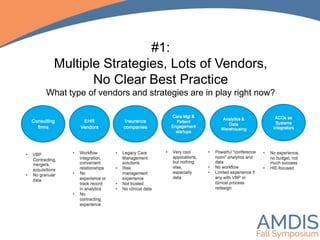
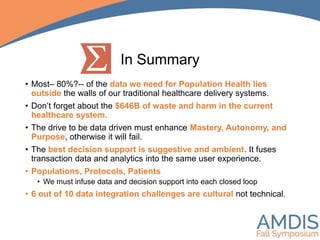
The document discusses the critical need for integrating external data sources to support decision-making in population health while emphasizing the importance of a human-centered approach to data utilization. It outlines the challenges organizations face in this integration, such as data governance and access to information systems, and advocates for suggestive analytics that enhance clinician decision-making. Ultimately, it highlights that 80% of relevant data for population health is outside traditional healthcare systems, and efforts must focus on addressing cultural challenges to effectively drive data integration.