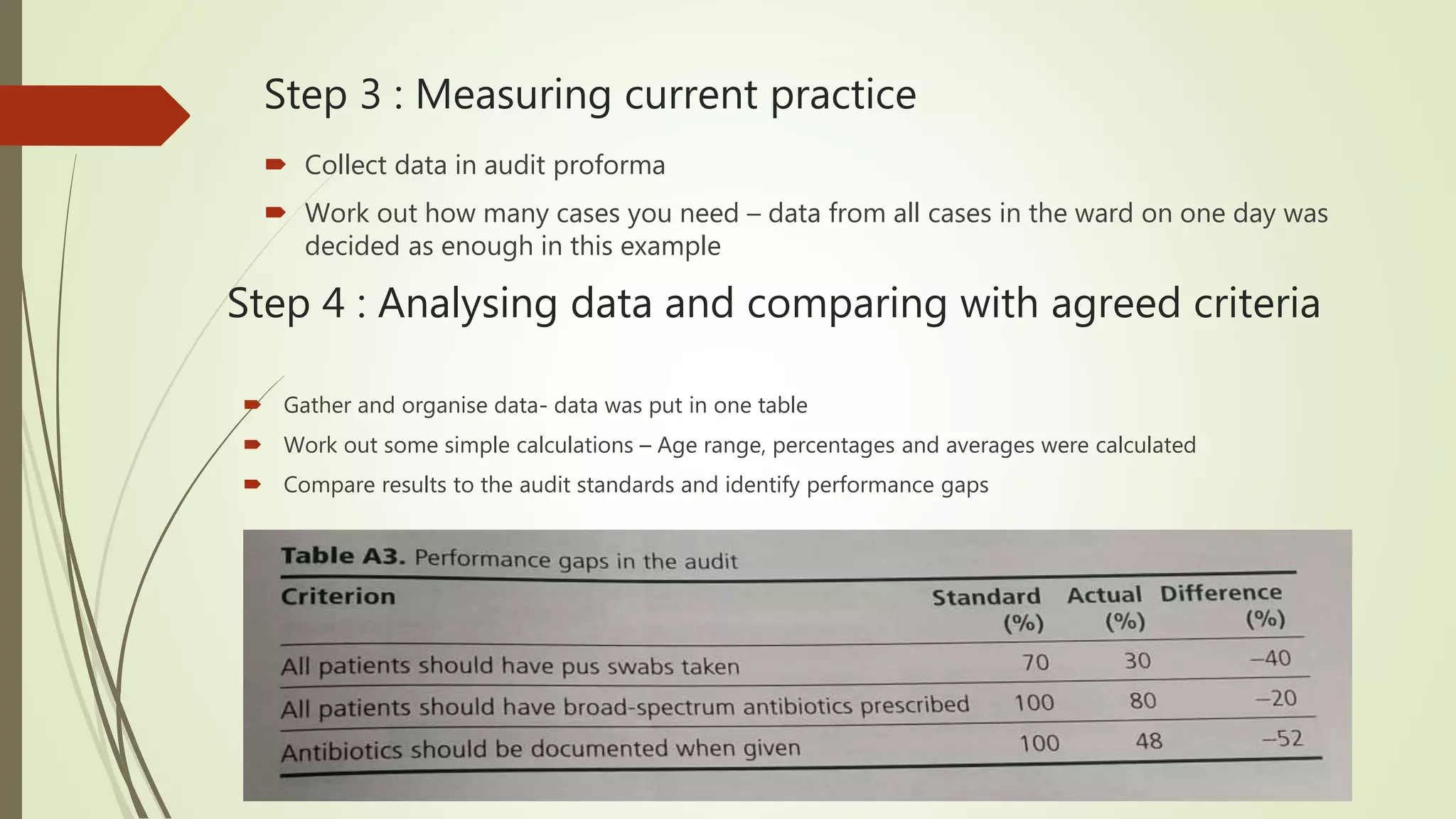
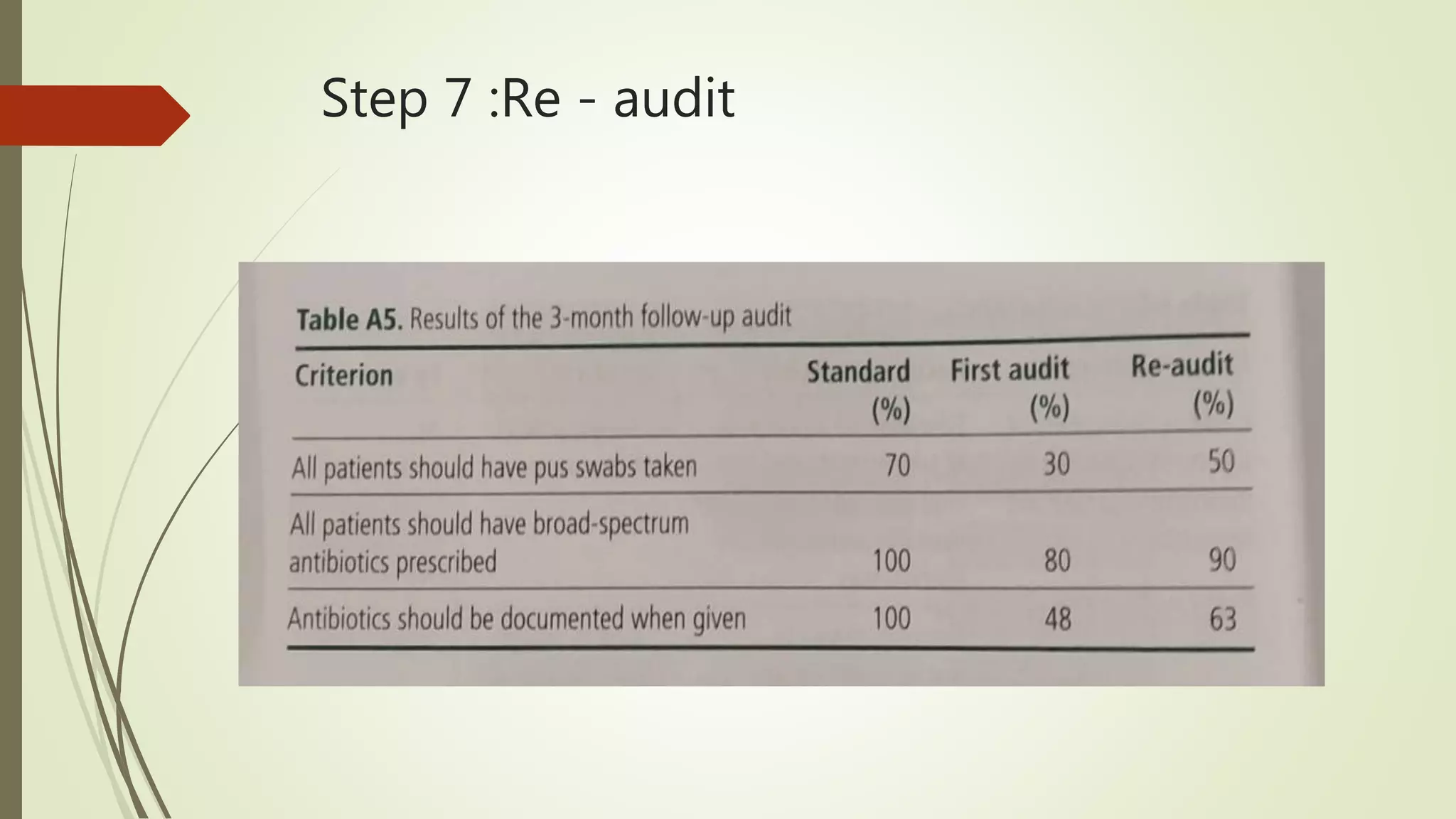
This document outlines the clinical audit process. It defines audit as reviewing, monitoring, and evaluating care against agreed standards to improve patient outcomes, use of resources, education, and staff reflection. Research aims to discover new information rather than evaluate existing care. The audit cycle involves identifying issues, setting criteria, measuring current practice, analyzing data against criteria, implementing changes, and re-auditing. Types of audits include structure, process, and outcome audits. Steps of the audit cycle are also demonstrated through an example audit on postoperative wound infections.