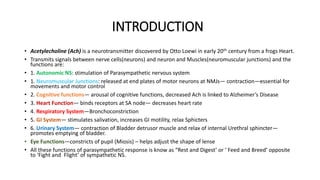
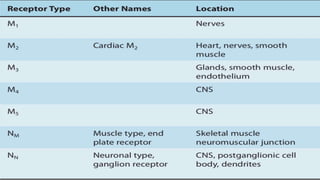
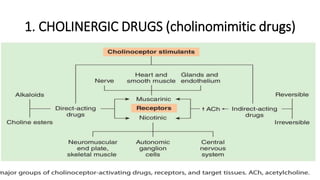
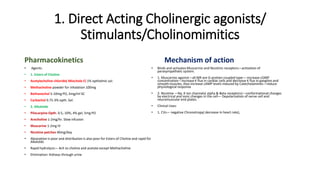
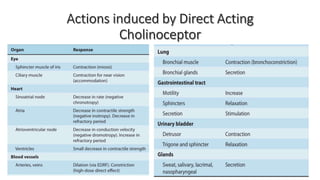
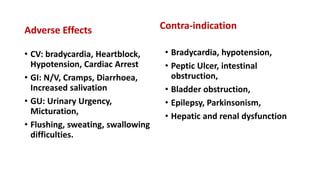
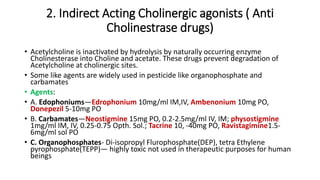
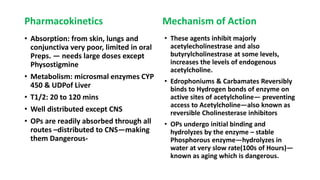
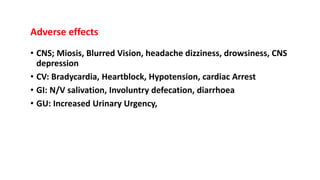
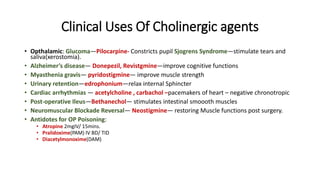
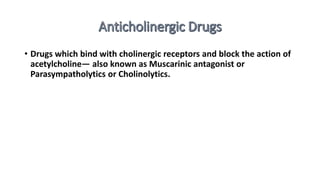
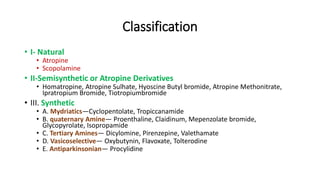
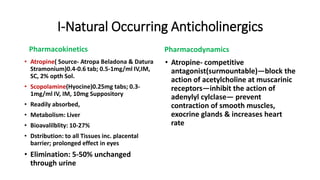
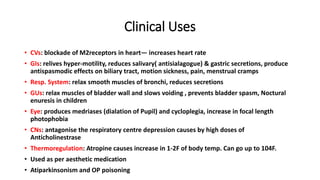
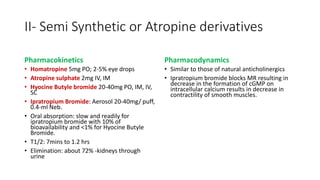
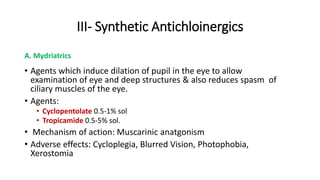
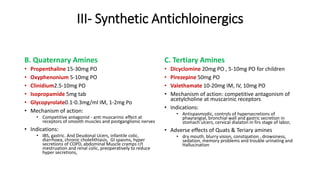
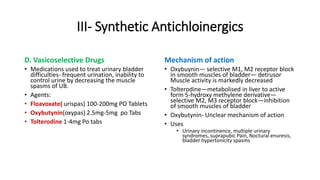
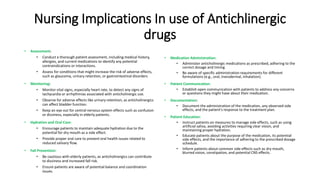
Acetylcholine is a neurotransmitter that functions in the autonomic nervous system, neuromuscular junctions, and cognitive processes. It binds to muscarinic and nicotinic receptors to stimulate parasympathetic responses. There are two main types of cholinergic drugs: direct-acting cholinergic agonists that mimic acetylcholine, and indirect-acting drugs that inhibit acetylcholinesterase to increase endogenous acetylcholine levels. Anticholinergic drugs act as competitive antagonists at muscarinic receptors to block acetylcholine's effects. They are used to treat various conditions by reducing parasympathetic activity.