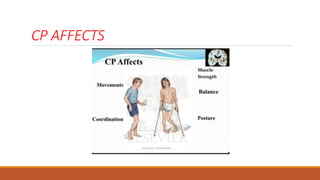
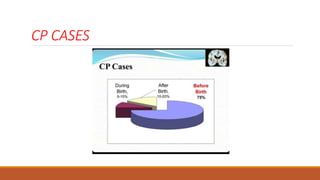
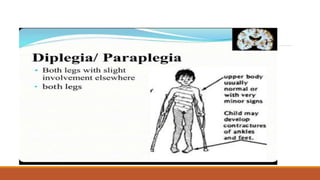
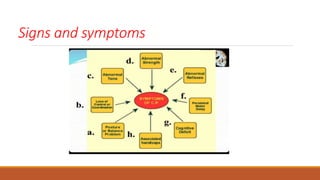
This document discusses evidence based recent research on play and children with cerebral palsy (CP). It provides information on CP, including that it is a motor function disorder caused by permanent brain damage. It describes the types and causes of CP and discusses associated problems. The document outlines assessments and treatments for CP, including physical, occupational and speech therapies. It defines play, discusses the benefits of play for children with CP, and describes different types of toys that can be used to facilitate play.