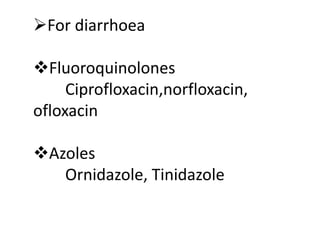
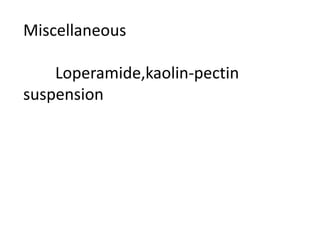
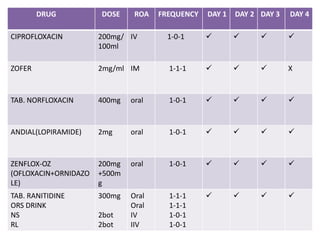
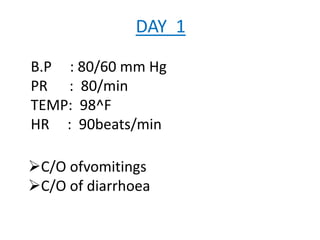
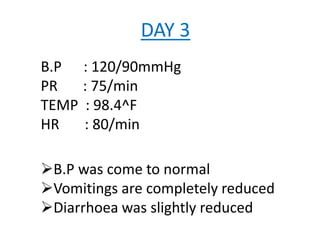
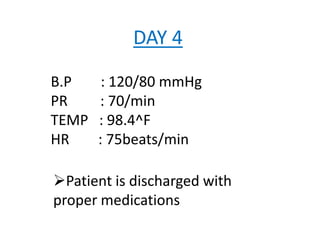
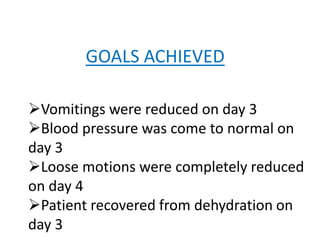
This document presents a case study of a 42-year-old male patient admitted with cholera. He presented with severe diarrhea for two days, vomiting for one day, and loss of skin elasticity and low blood pressure. Examination of a stool sample under a microscope confirmed the presence of Vibrio cholerae bacteria. He was treated with IV and oral rehydration, antibiotics, and antiemetics. His condition improved over four days of treatment, with blood pressure and symptoms normalizing before discharge with medications and counseling.