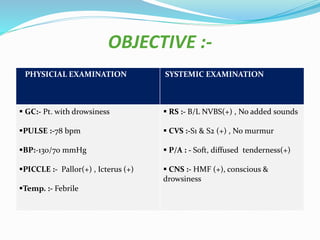
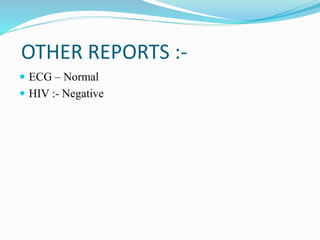
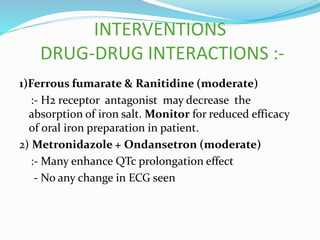
A 50-year-old male was admitted with swelling of the lower limbs, fever, chills, vomiting, and diarrhea. He has a history of chronic kidney disease and malaria. On examination, he was febrile and had pallor, icterus, and tenderness in the abdomen. Laboratory tests showed decreased hemoglobin and kidney function. He was diagnosed with chronic kidney disease exacerbation and malaria and treated with IV fluids, antibiotics, antimalarials, and other medications. His condition improved and he was discharged on medications including antibiotics and supplements with counseling on diet, lifestyle and medication adherence.