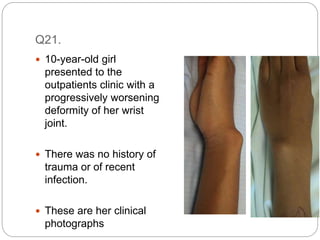
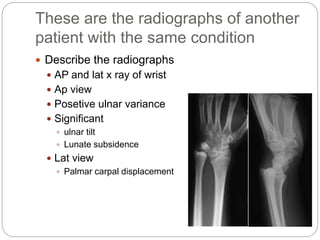
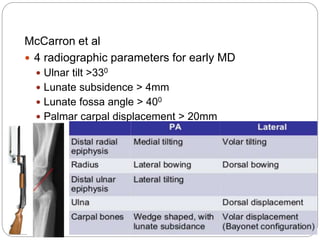
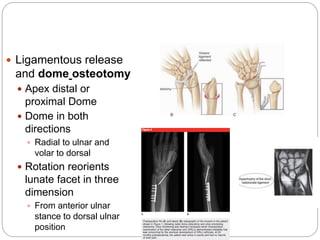
This document discusses the case of a 10-year-old girl presenting with a progressively worsening wrist deformity with no history of trauma or infection. Radiographs show features characteristic of Madlung deformity, including positive ulnar variance, ulnar tilt, and lunate subsidence. Madlung deformity results from abnormal growth of the distal radial physis. Treatment depends on severity of deformity and symptoms, and may include conservative management for mild cases or surgical correction such as dome osteotomy for more severe cases. The goals of surgery are pain relief, correction of deformity, and increased range of motion.