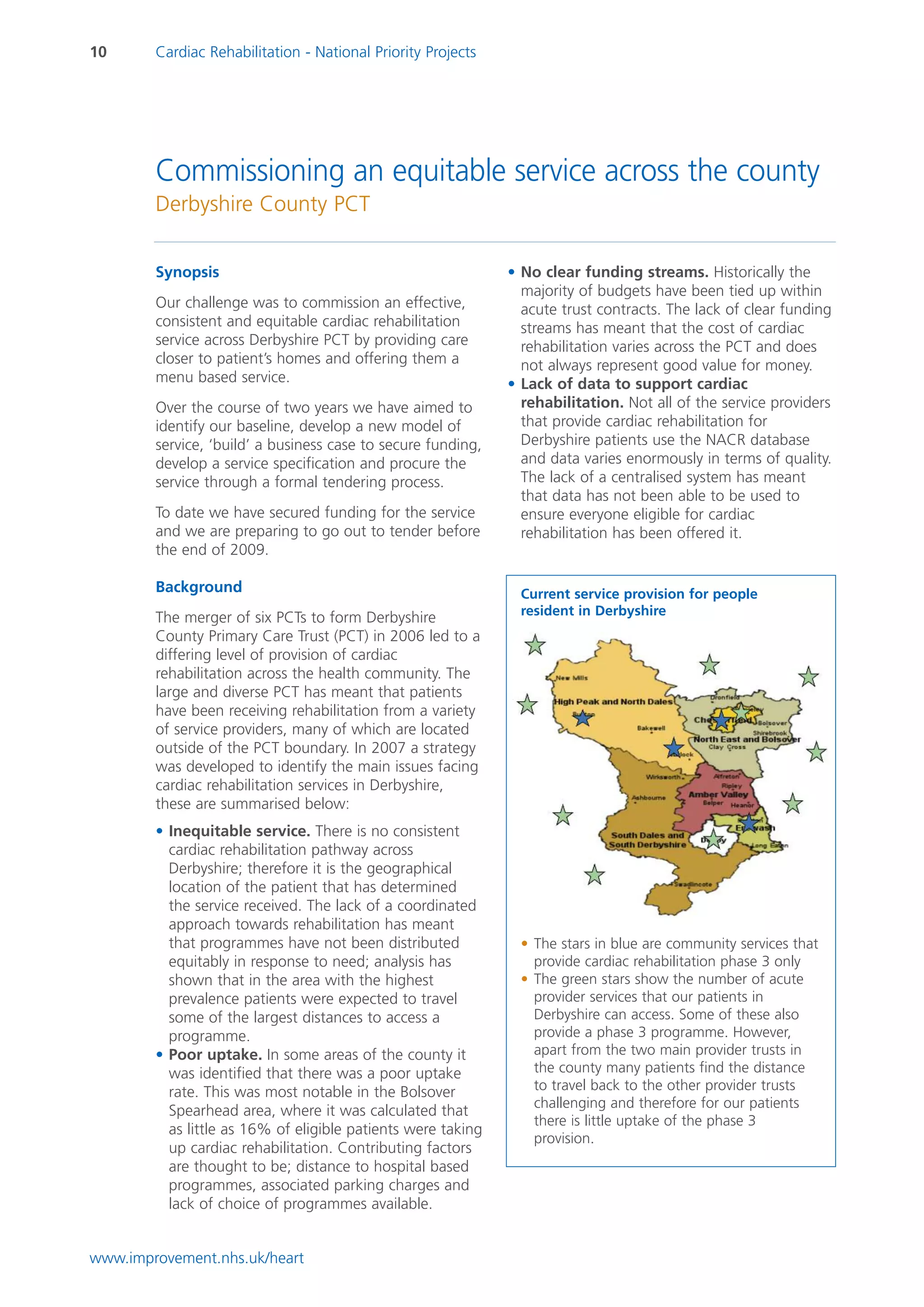
The document outlines the NHS Improvement's national priority projects for cardiac rehabilitation, aiming to enhance access, equity, and uptake of services for patients with heart conditions. Key lessons learned include the importance of strong clinical leadership, effective data use, and engaging stakeholders, which have been instrumental in driving improvements in service provision. Additionally, the document emphasizes addressing inequalities and enhancing patient choice in rehabilitation services while tackling the challenges of funding and service consistency.