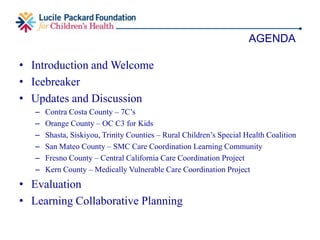
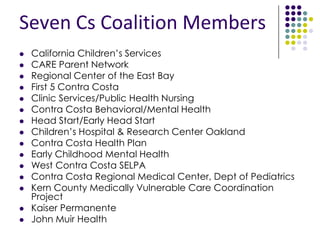
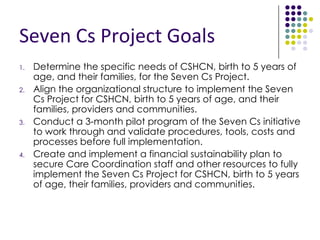
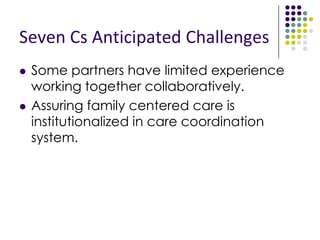
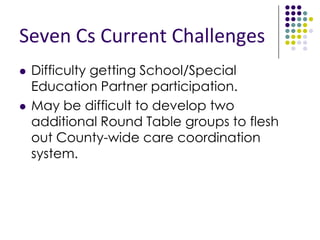
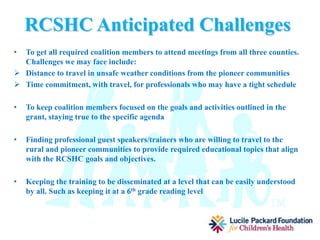
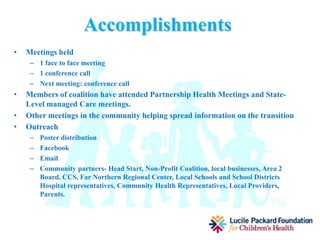
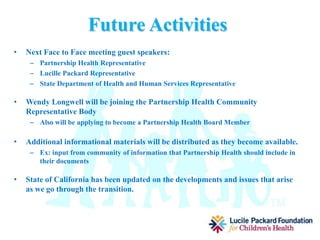
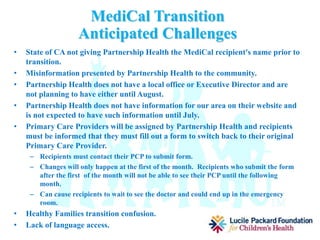
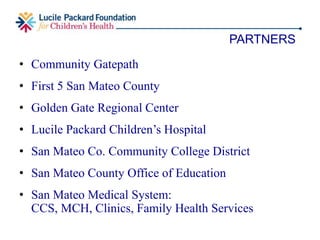
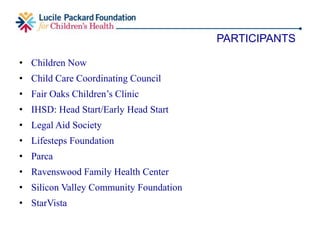
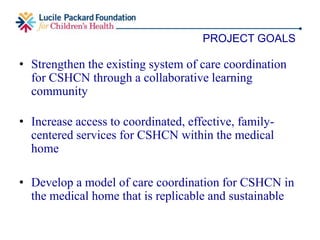
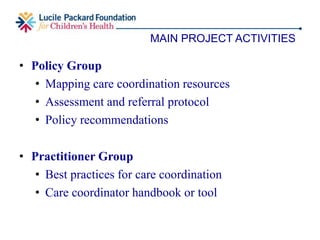
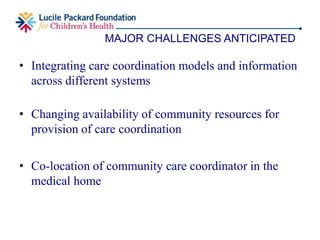
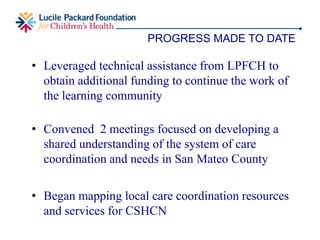
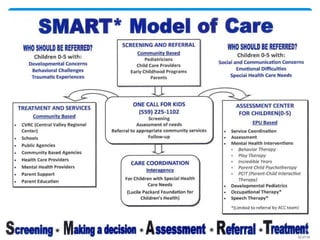
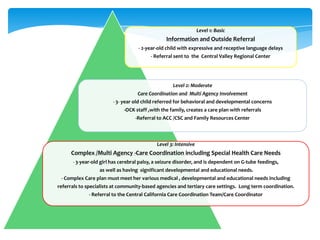
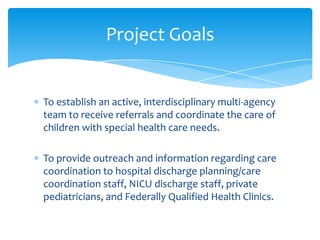
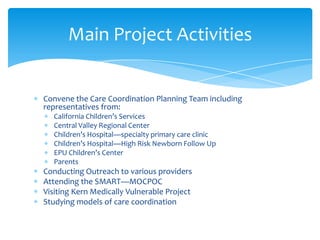
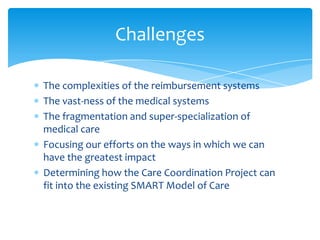
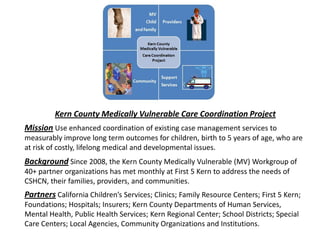
The document outlines various initiatives focused on community care coordination for children with special health care needs (CSHCN) in California, detailing specific projects in counties like Contra Costa, Orange, and Kern. Each project's goals include assessing community needs, developing care coordination systems, and implementing sustainable plans while addressing challenges such as collaboration among partners and resource limitations. Collaborative efforts involve multiple stakeholders from health services, education, and family support networks aiming to improve health outcomes and provide comprehensive care for families with CSHCN.