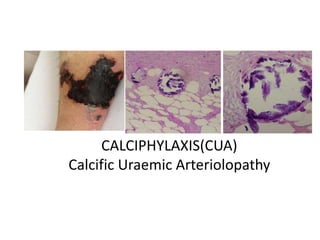
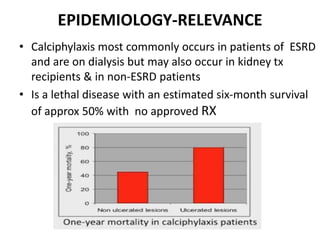
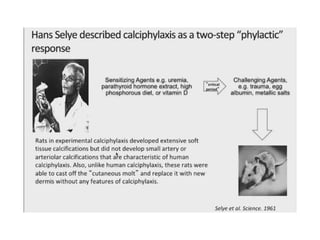
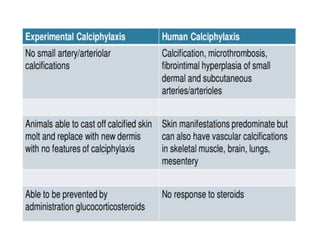
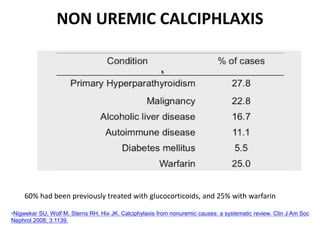
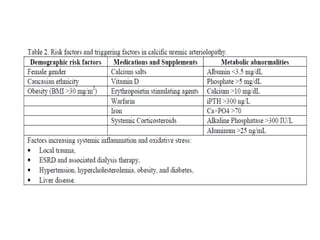
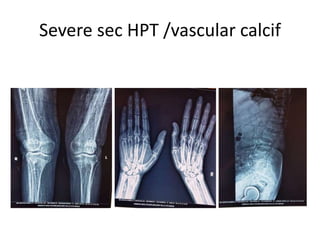
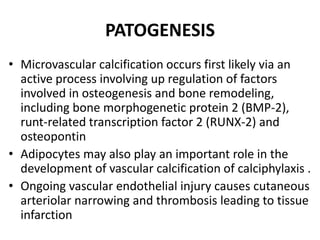
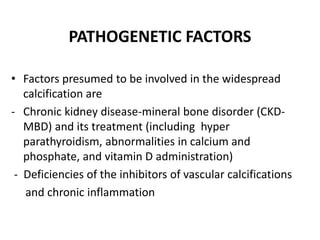
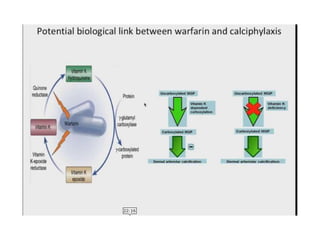
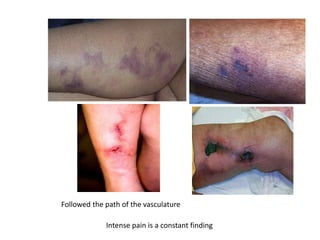
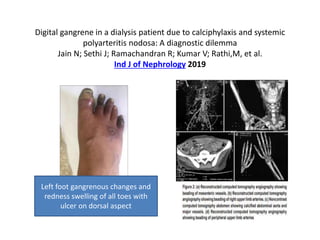
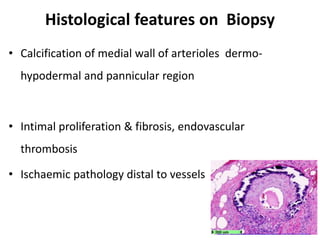
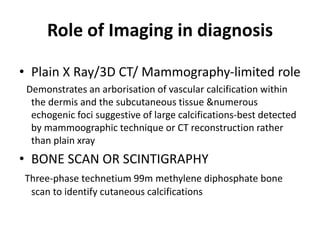
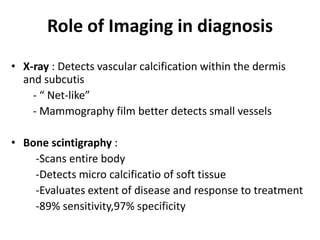
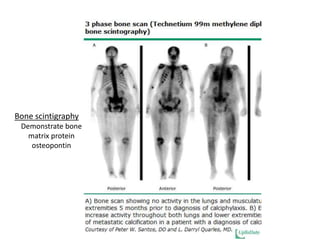
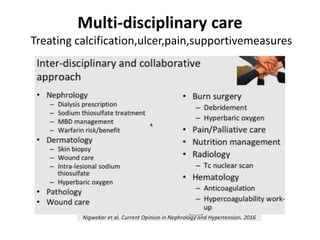
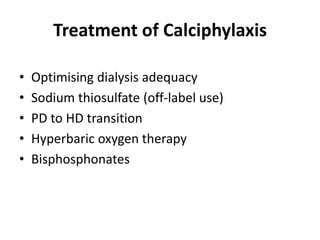
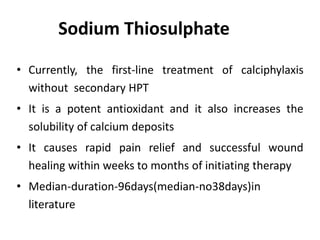
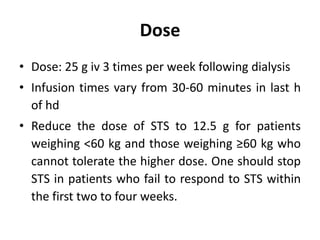
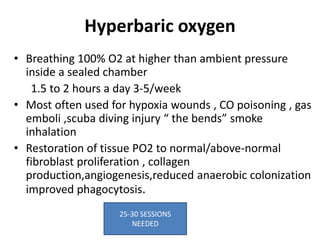
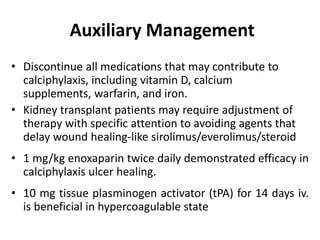
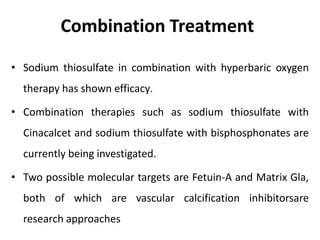
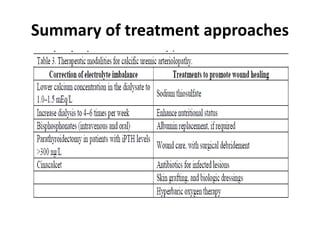
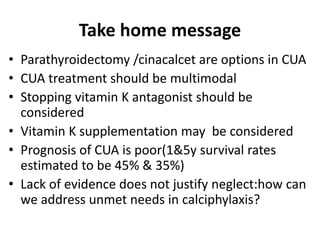
Calciphylaxis, also known as calcific uremic arteriolopathy, is a rare disorder characterized by calcification of the small blood vessels of the skin and subcutaneous fat. It most commonly occurs in patients with end-stage renal disease on dialysis. The calcification leads to reduced blood flow and painful skin lesions. Risk factors include hyperparathyroidism, vitamin D use, and warfarin use. Diagnosis is made clinically and confirmed with biopsy showing vessel calcification. Treatment involves sodium thiosulfate, hyperbaric oxygen, bisphosphonates, and wound care. Prognosis is poor with high mortality rates due to complications like infection and organ failure.