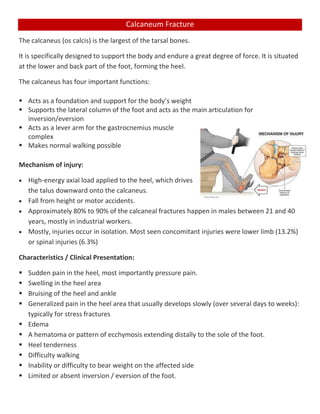
The calcaneus is the largest tarsal bone in the foot and acts as the foundation and lever for the foot and lower leg. Calcaneus fractures most commonly occur from high-energy impacts to the heel that drive the talus down onto the calcaneus. They present with pain and swelling in the heel and difficulty walking. Treatment depends on the fracture type but often involves initial immobilization, physical therapy to regain range of motion and strength, and progression to full weight bearing over several months to allow healing. Surgical fixation may be required for displaced fractures to realign the bones.
![Azhaan Mohammad Asiad
17SMAS101050 [Galgotias University]
[CALCANEUM FRACTURE]](https://image.slidesharecdn.com/calcaneumfracture-200620055818/85/Calcaneum-fracture-1-320.jpg)