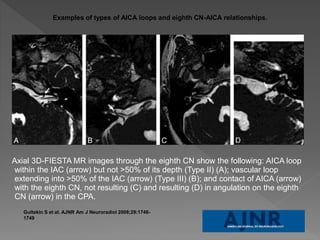
- Neurovascular compression syndrome (NVCS) refers to nerve compression by aberrant or tortuous blood vessels, which can cause cranial nerve dysfunction including trigeminal neuralgia.
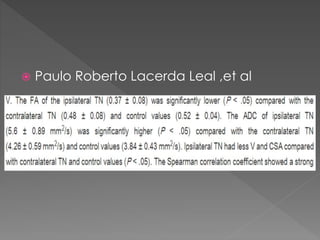
- Trigeminal neuralgia is characterized by abrupt, unilateral facial pain and is most often caused by neurovascular compression of the trigeminal nerve at the root entry/exit zone from the brainstem.
- MRI with techniques like CISS and MRA-TOF are effective in evaluating neurovascular relationships and compressions, aiding surgical planning for microvascular decompression to treat refractory trigeminal neuralgia.