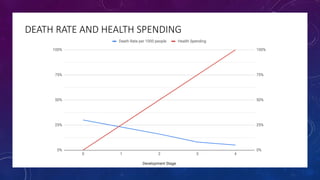
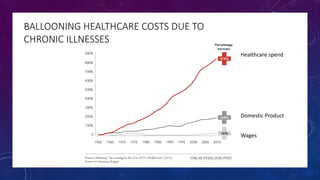
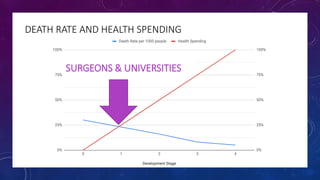
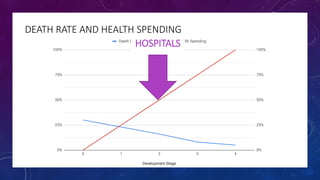
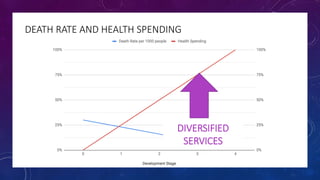
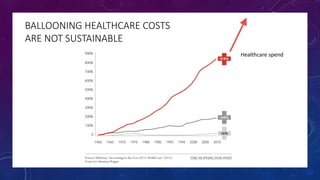
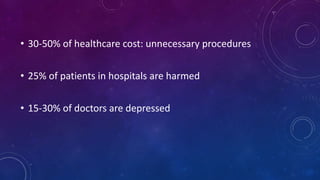
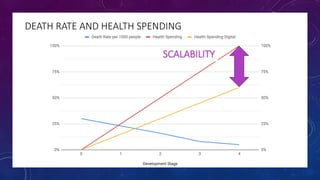
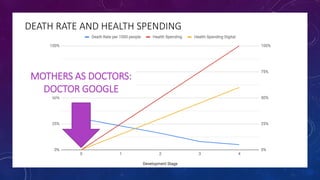
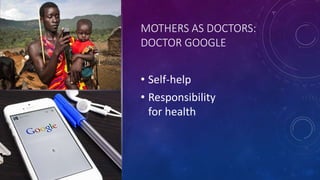
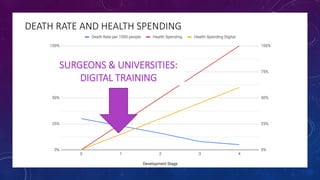
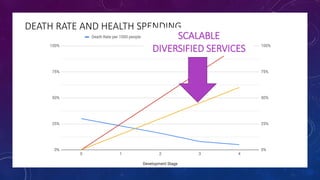
The document discusses building a new healthcare system from scratch using modern technologies and principles. It argues that existing systems focus too much on treating sickness rather than maintaining health. A new system would use technologies like telehealth, machine learning, and drones to scale healthcare access and education by empowering individuals to take responsibility for their own health. Key aspects would include virtual doctor visits, at-home recovery after outpatient clinics replace hospitals, and empowering people with health information through platforms like "Doctor Google". The goal is an affordable, scalable system that promotes equitable access to healthcare worldwide.