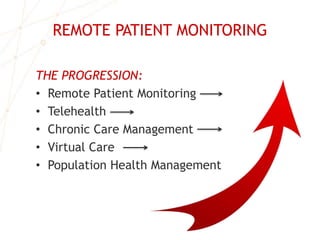
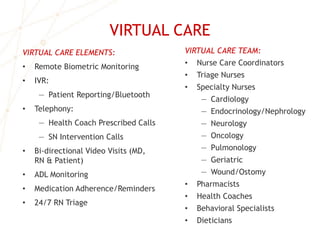
This document summarizes the business case for remote patient monitoring. It outlines how remote monitoring has progressed from initial technologies to integrated virtual care solutions. It shows how new care delivery models incentivize providers to adopt remote monitoring to reduce costs and improve outcomes. Studies show remote monitoring can significantly reduce hospitalizations, ER visits, and costs for patients with chronic conditions. The document concludes by describing opportunities for hospitals, physicians, and post-acute providers to leverage remote monitoring.