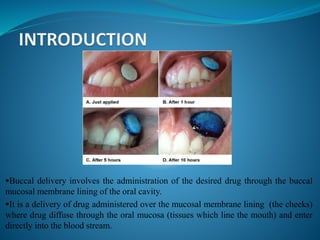
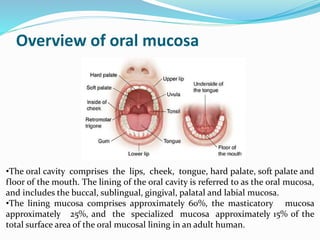
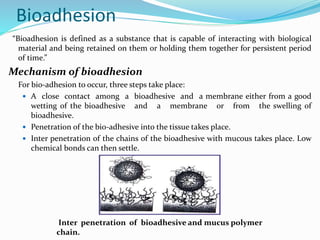
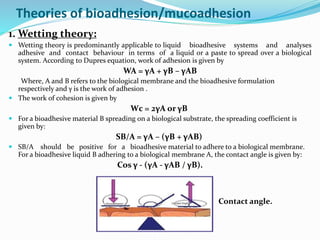
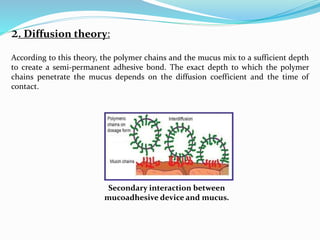
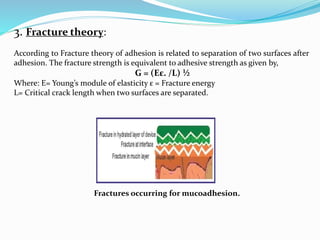
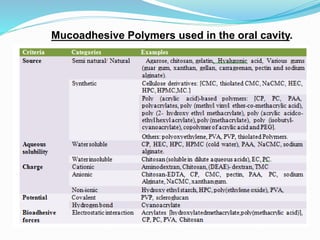
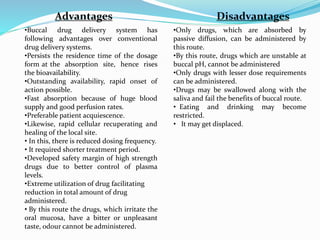
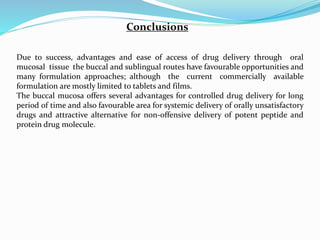
This document discusses buccal drug delivery, which involves administering drugs through the buccal mucosa in the mouth. It provides an overview of the oral mucosa and its components. Bioadhesion and the theories behind it, such as wetting, diffusion, fracture, and adsorption theories are explained. Factors affecting bioadhesion like polymer properties and environment are outlined. The basic components of buccal drug delivery systems including suitable drug substances, bioadhesive polymers, backing membranes, and permeation enhancers are described. Examples of mucoadhesive polymers and permeation enhancers are given. Buccal drug delivery offers advantages over other routes like increased bioavailability and reduced dosing frequency.