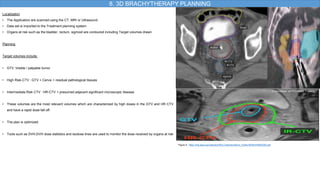
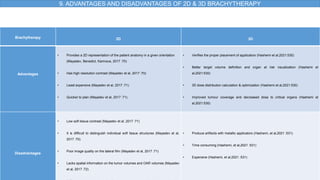
This document discusses 2D and 3D brachytherapy planning. It begins with an introduction and overview of brachytherapy applications and indications for gynecological cancers. It then covers 2D brachytherapy planning which uses X-rays and fluoroscopy for applicator placement verification and dose calculations. 3D brachytherapy planning utilizes CT, MRI and ultrasound for target and organ at risk delineation and advanced 3D dose optimization. The advantages of 3D planning include improved tumor coverage and reduced doses to organs at risk compared to 2D planning which provides only a basic 2D representation of anatomy.