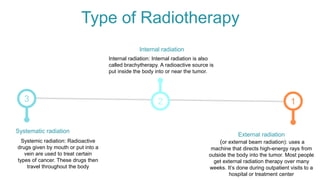
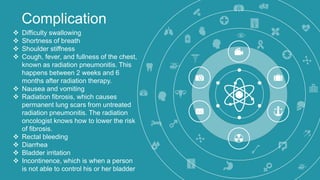
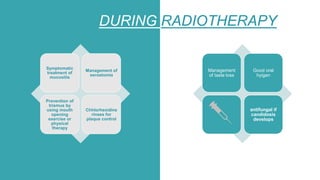
Radiotherapy is a common cancer treatment that uses beams of intense energy to kill cancer cells. It can be delivered externally via machine or internally via radioactive sources placed near the tumor. The main goals are to shrink tumors and kill cancer cells. Common oral complications include mucositis, infections, xerostomia, and trismus. Management involves preventative dental work before treatment, symptomatic care during, and frequent follow ups after to monitor for late effects like osteoradionecrosis.