This document summarizes evidence on blood product transfusions in critically ill children. Key points include:
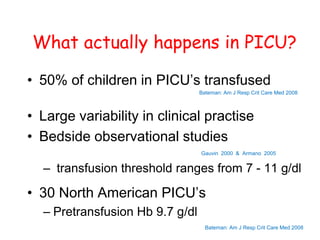
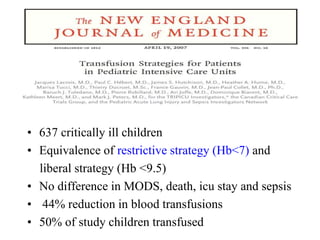
- About 50% of children in pediatric intensive care units (PICUs) receive red blood cell transfusions, though transfusion practices vary significantly between hospitals and bedside practices.
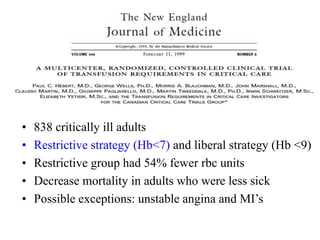
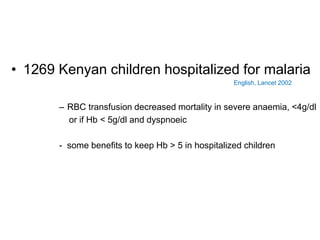
- Evidence supports a restrictive transfusion strategy (transfusing when hemoglobin is <7 g/dL) over a liberal strategy (<9.5 g/dL), as restrictive use reduces transfusions by 44% without increasing adverse outcomes.
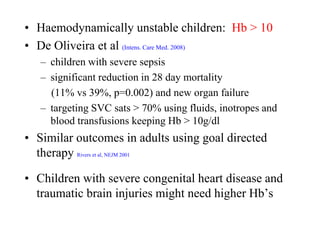
- For unstable children, such as those with severe sepsis, targeting a hemoglobin >10 g/dL through transfusions and other interventions may reduce mortality compared to lower hemoglobin levels.
-