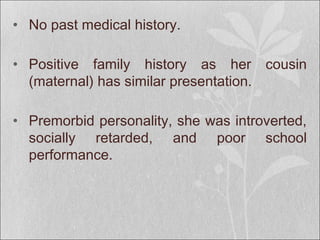
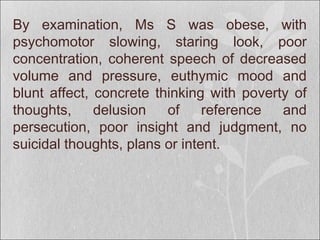
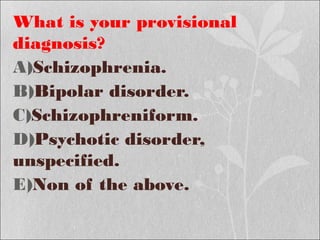
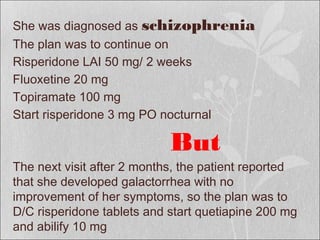
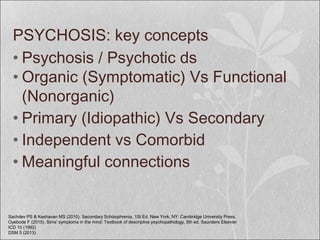
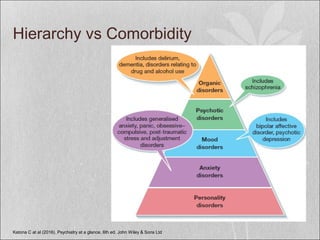
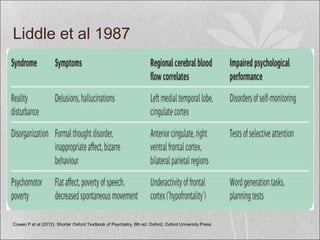
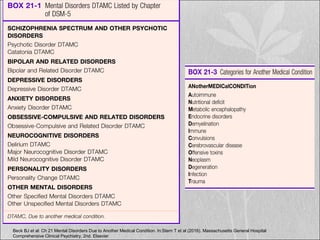
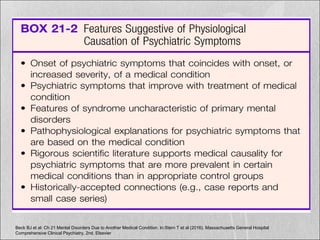
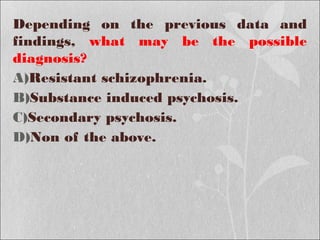
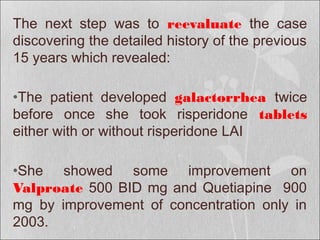
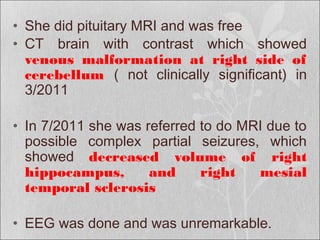
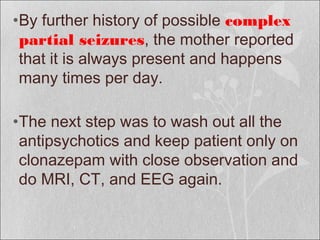
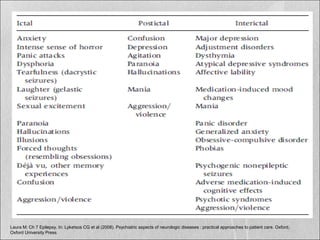
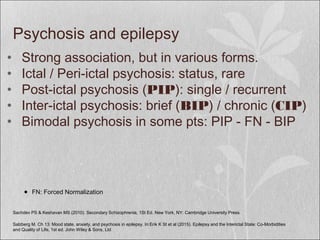
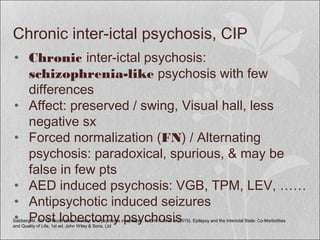
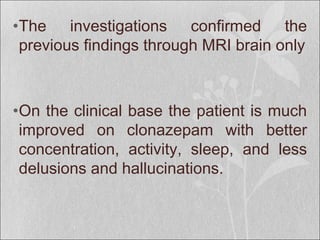
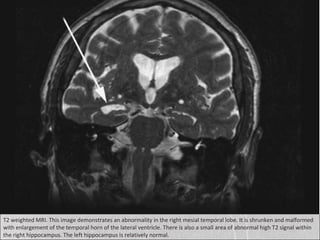
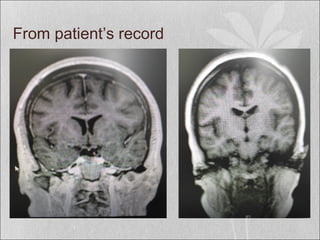
This case presents a 32-year-old female with a long history of psychotic symptoms including auditory hallucinations, delusions, disorganized behavior, and mood changes. Her symptoms did not respond well to various antipsychotic treatments. Further history revealed complex partial seizures. Imaging showed right mesial temporal sclerosis. After discontinuing antipsychotics and treating only with antiepileptics, her symptoms improved, suggesting her psychosis was likely secondary to her underlying epilepsy from mesial temporal sclerosis rather than a primary psychotic disorder. Mesial temporal sclerosis is a common cause of treatment-resistant epilepsy and associated interictal psychosis.