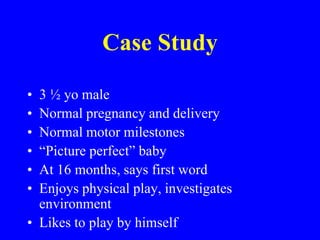
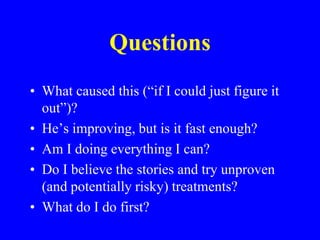
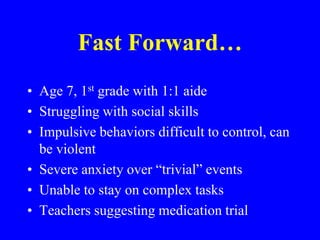
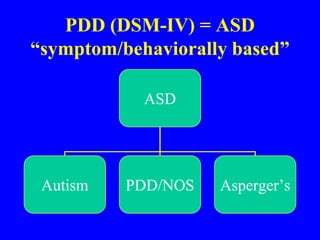
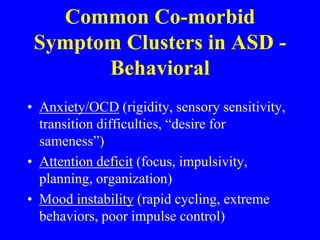
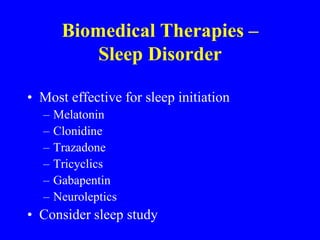
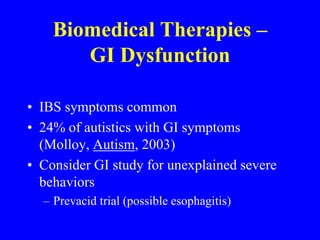
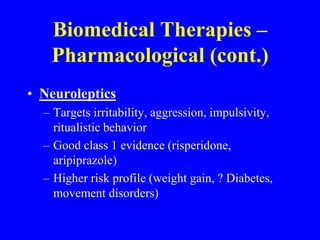
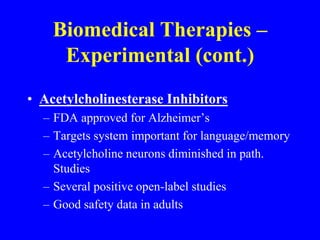
This document provides an overview of biomedical therapies for autism, including dietary modifications, supplements, pharmacological interventions, and experimental treatments. It presents a case study of a child diagnosed with autism and discusses the family's questions. It then outlines 10 rules for considering biomedical therapies, emphasizing that they should not replace behavioral therapies and have limited evidence for treating core autism symptoms. Various therapy options are described along with theories for their mechanisms and potential benefits and risks. Experimental therapies with little evidence are also mentioned.