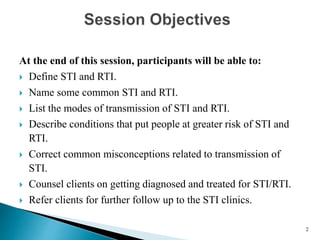
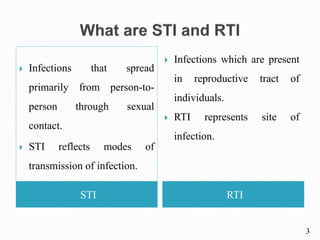
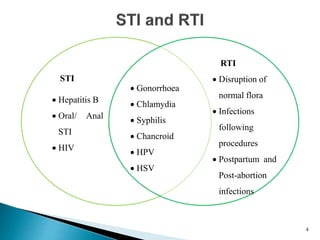
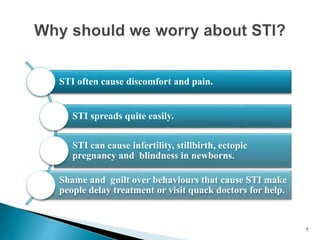
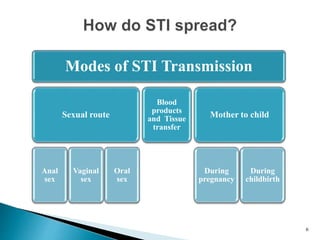
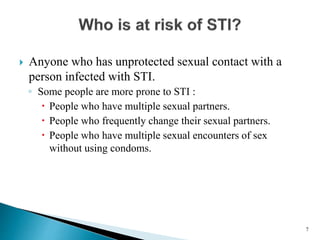
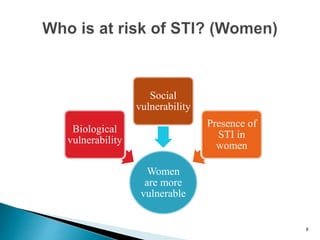
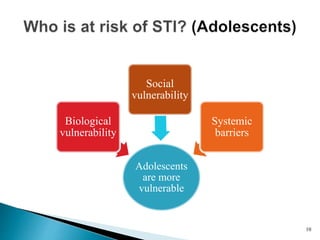
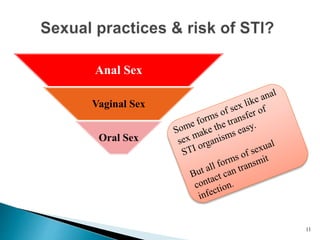
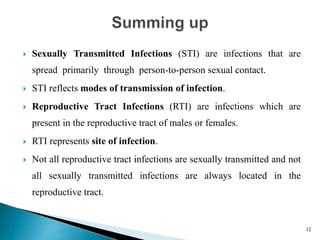
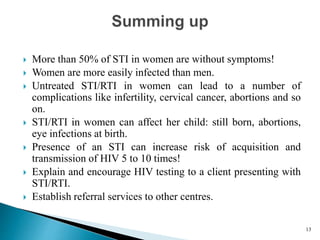
This document outlines topics that participants will learn about related to sexually transmitted infections (STI) and reproductive tract infections (RTI). It defines STI as infections spread through sexual contact while RTI refers to infections located in the reproductive tract. Common STIs and RTIs are listed along with their modes of transmission. Conditions that increase risk of infection are described, such as having multiple partners or unprotected sex. The document emphasizes that women are more vulnerable biologically and socially to STI/RTI and that untreated infections can lead to complications like infertility. It stresses counseling clients without judgment and addressing misconceptions to ensure proper treatment and referral.