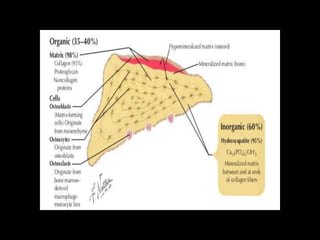
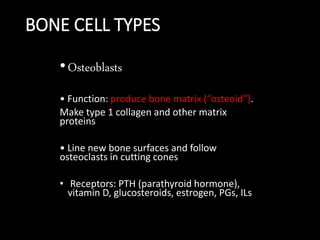
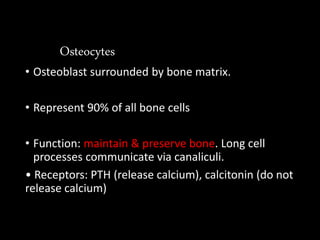
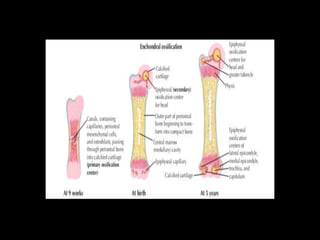
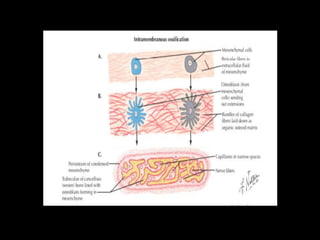
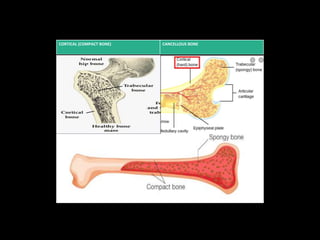
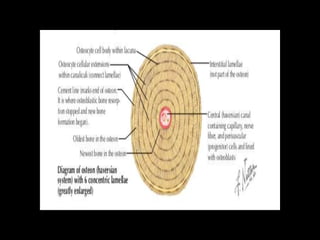
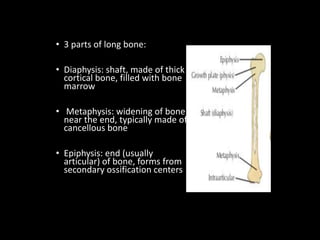
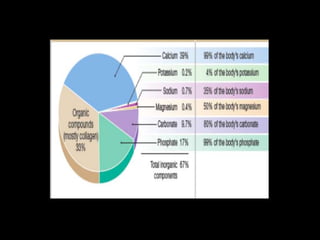
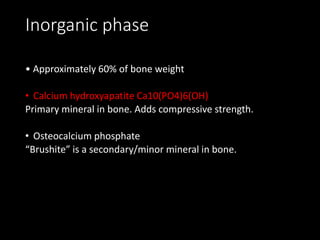
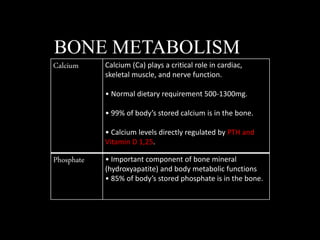
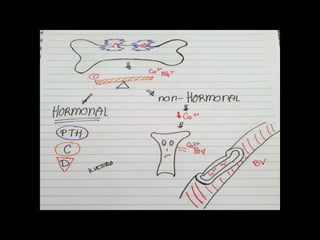
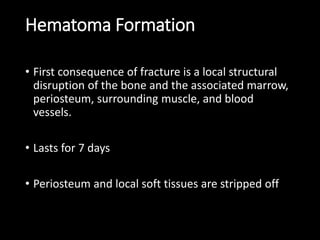
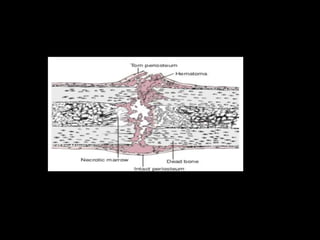
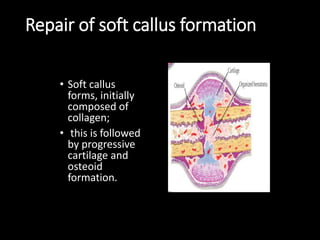
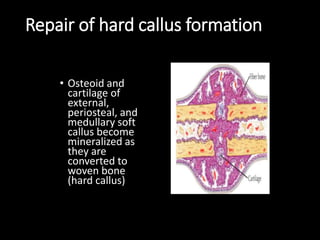
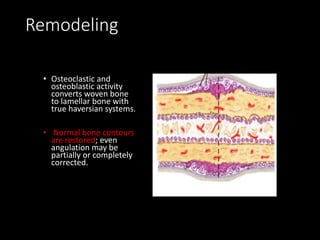
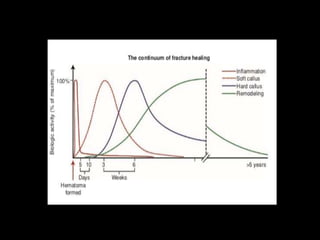
This document summarizes key information about bone structure, cells, formation, metabolism, and fracture repair. It describes that bone has structural and reservoir functions, is remodeled through modeling and remodeling, and contains osteoblasts, osteocytes, and osteoclasts. Bone formation occurs through endochondral, intramembranous, or appositional ossification. Fracture repair involves hematoma formation, soft callus formation, hard callus formation, and remodeling to restore bone structure.