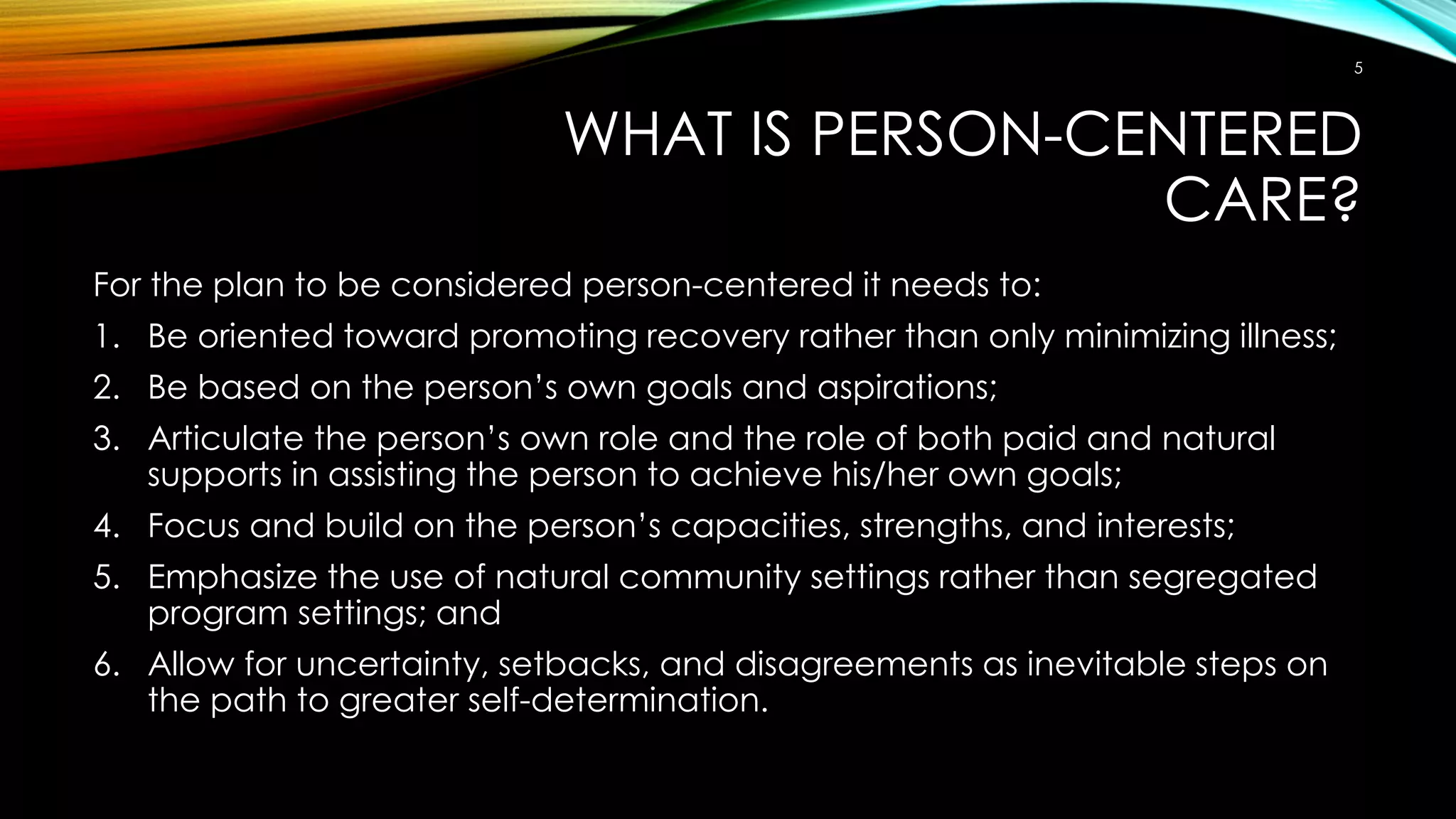
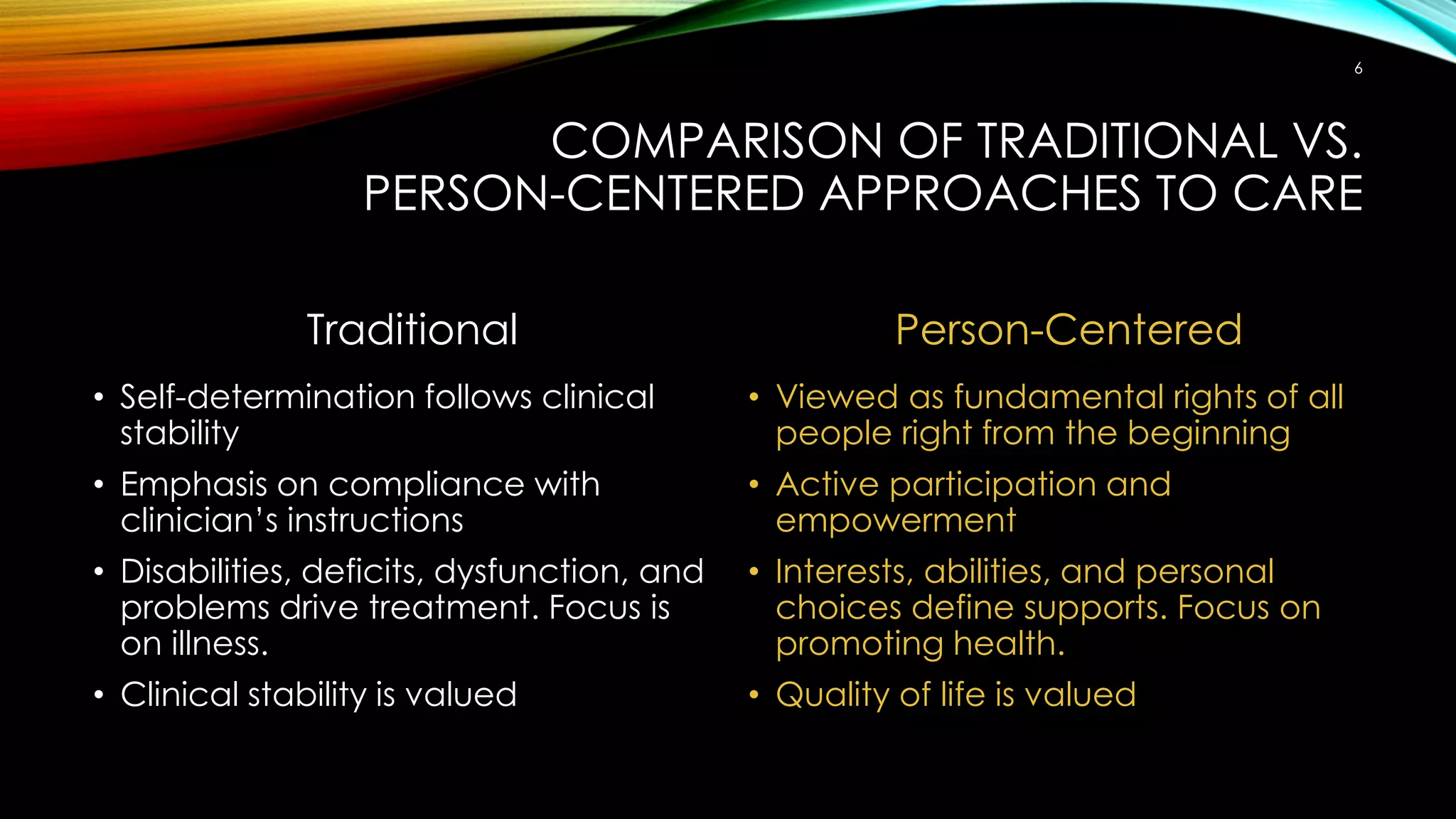
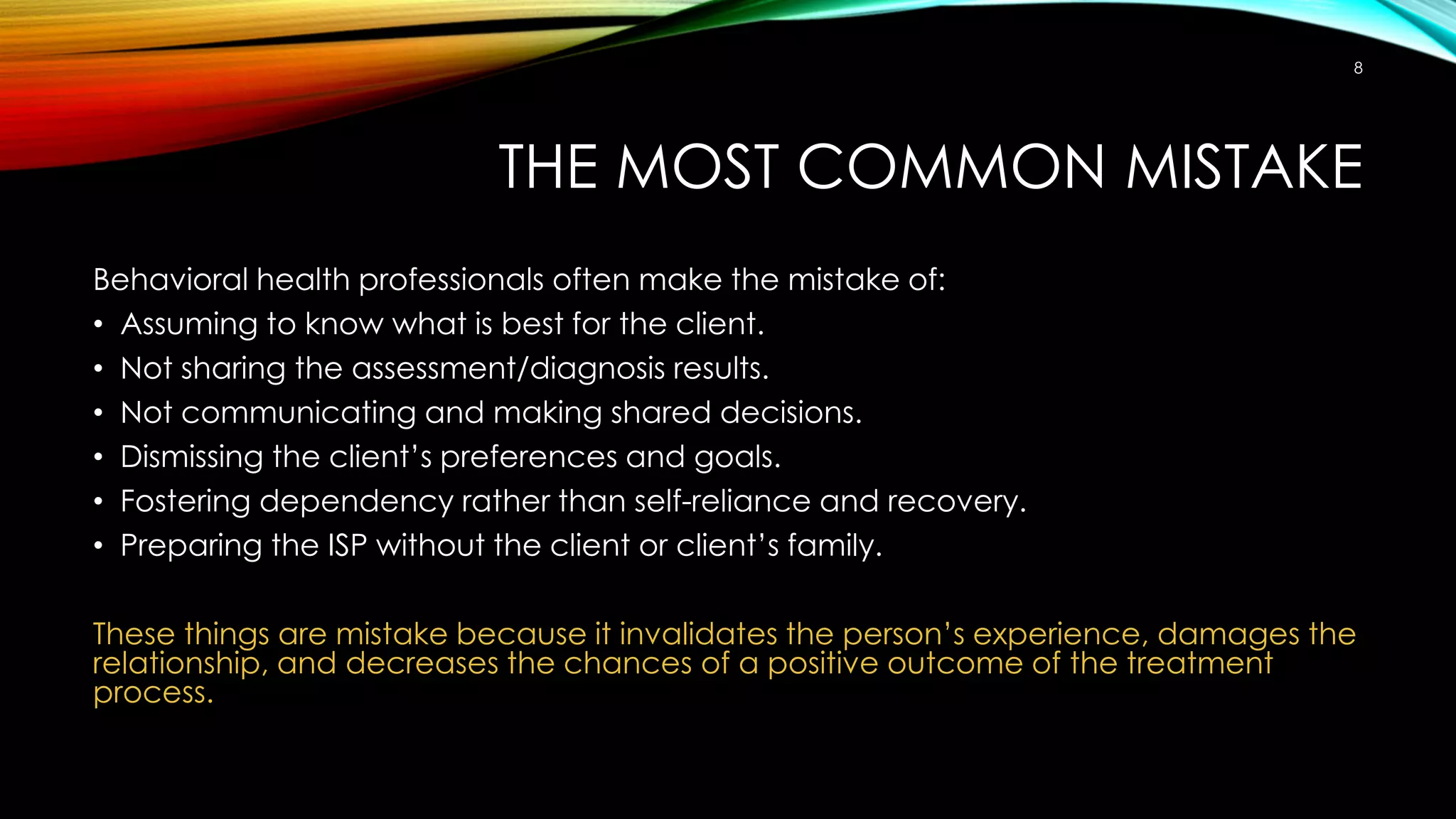
The document discusses the principles of person-centered care and treatment planning. It emphasizes that person-centered care (1) promotes recovery over illness minimization, (2) is based on the individual's own goals and choices, and (3) involves collaborative decision-making between the individual and their supports. In contrast, traditional treatment focuses on compliance, deficits, and clinical stability rather than self-determination and quality of life. The most common mistake made is assuming the provider knows best rather than including the individual. Person-centered practice speaks in strengths-based terms, addresses barriers rather than pathologies, and views the individual-provider relationship as a partnership.