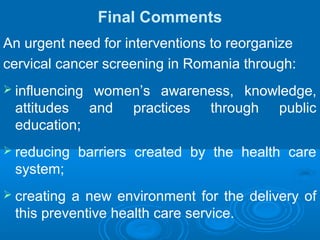
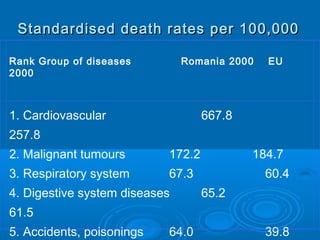
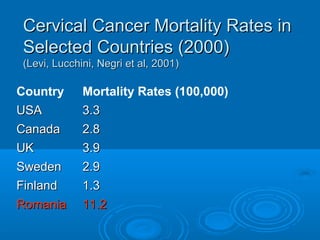
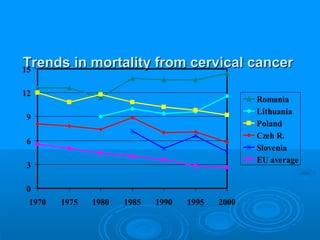
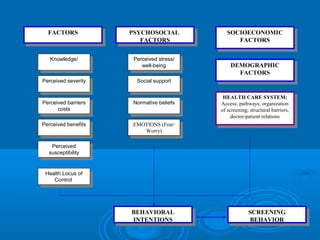
1) Romania has high rates of cervical cancer mortality compared to other European countries due to undervaluation of preventive care like Pap smears.
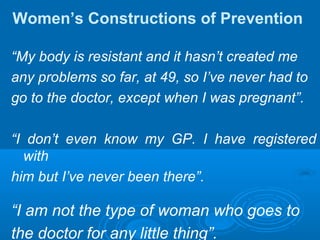
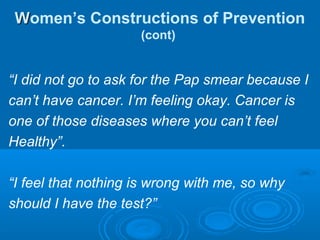
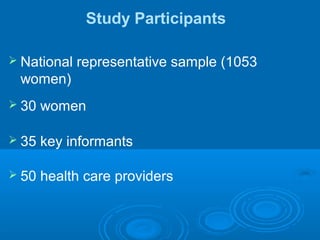
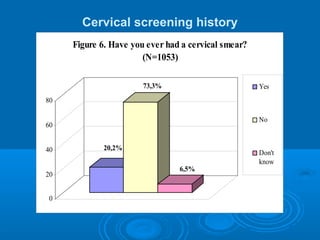
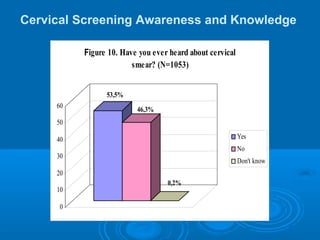
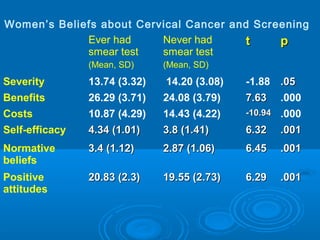
2) A study found that only 20% of Romanian women have ever had a Pap smear, with many lacking awareness or believing smears are unnecessary.
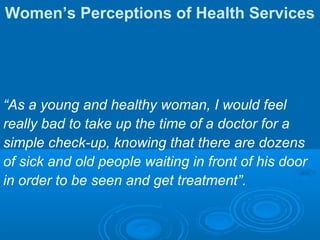
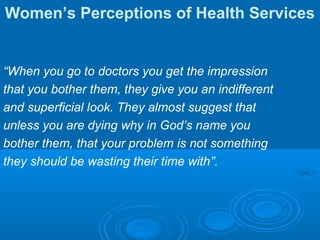
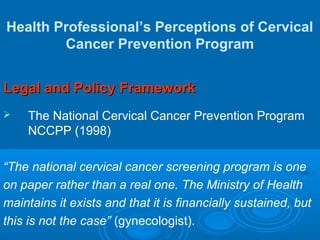
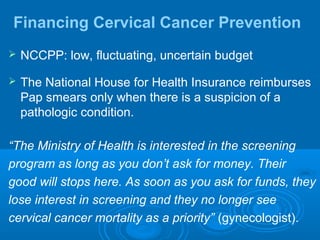
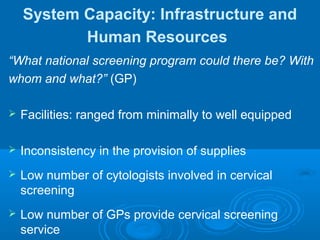
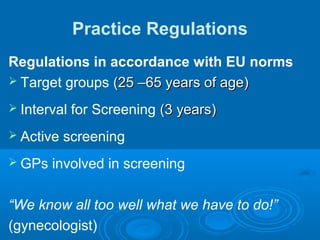
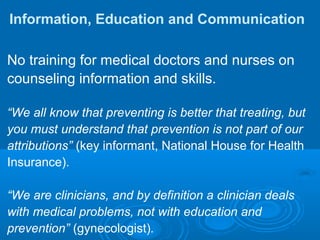
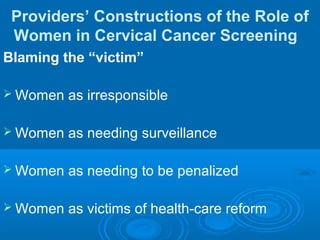
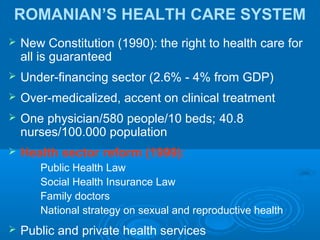
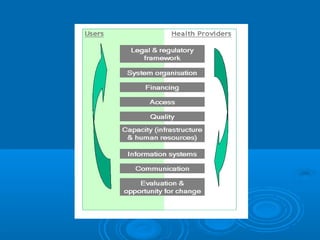
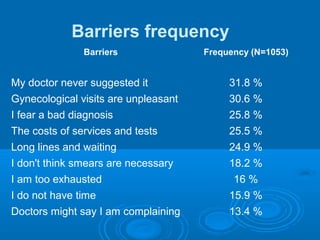
3) Barriers to screening included costs, fear of diagnosis, and perceptions that doctors are overburdened. The health system is underfunded and screening program exists only on paper.





![Predictors of Screening Behavior
Dimension Model 4
Residence*Residence* 1.90 [1.13-3.20]
KnowledgeKnowledge 1.58 [1.37-1.83]
Normative beliefsNormative beliefs 1.27 [1-1.61]
AgeAge 1.03 [1.00-1.05]
Perceived psychological costsPerceived psychological costs .88 [.83-.94]
Frequency of gynecologicalFrequency of gynecological
examsexams
.71 [.56-.90]
Marital status (married)Marital status (married) .35 [.14-.82]
Nagelkerke RNagelkerke R22
0.43](https://image.slidesharecdn.com/baban5-130722122745-phpapp02/85/What-Happens-When-Women-s-Preventive-Care-is-Undervalued-Lessons-from-Romania-21-320.jpg)