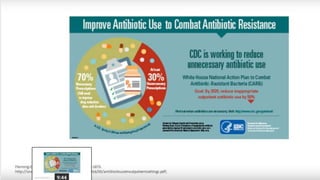
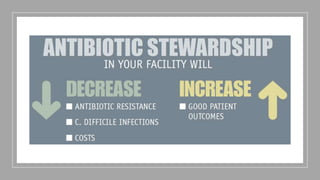
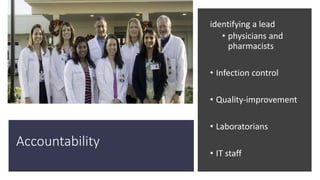
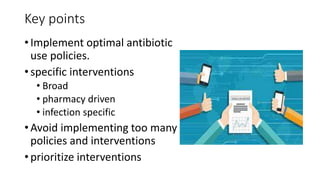
Antibiotic stewardship programs aim to optimize antibiotic use, improve patient outcomes, reduce antibiotic resistance and adverse events. They involve multidisciplinary teams who provide guidance and feedback on prescribing. Core elements include leadership commitment, accountability, drug expertise, tracking antibiotic use and resistance over time, and educating prescribers. Specific interventions target broad antibiotic use as well as infection-specific treatment protocols. Regular reporting and education helps ensure optimal antibiotic stewardship.