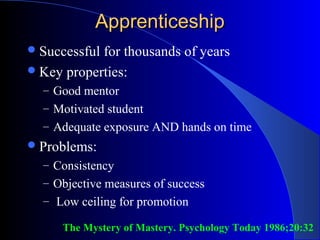
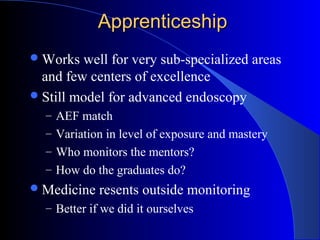
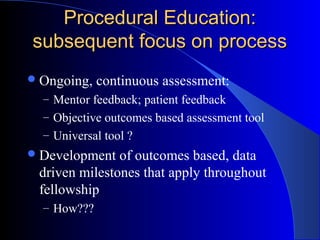
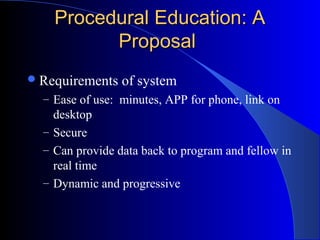
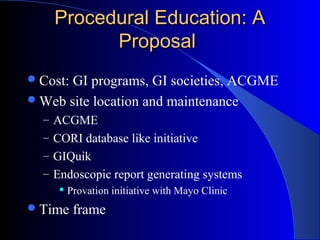
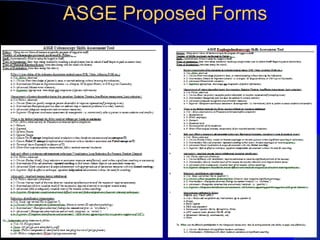
The document discusses procedural assessment in gastroenterology training. It outlines the limitations of prior apprenticeship and competency-based models, and argues that outcomes-based learning focusing on milestones is needed. It proposes developing universal assessment tools, web-based submission of evaluations, and data-driven milestones to standardize procedural training across programs. Barriers like integrating assessments and overcoming silos must be addressed for successful implementation.