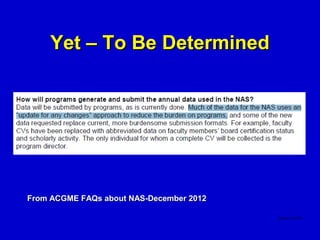
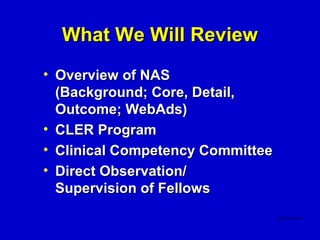
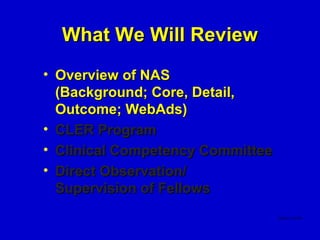
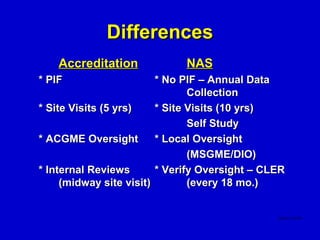
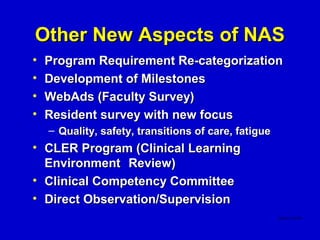
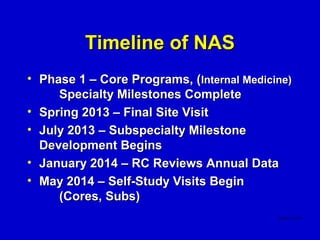
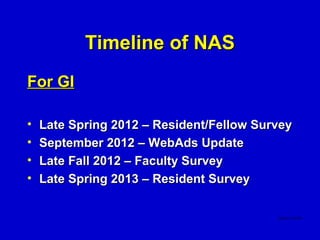
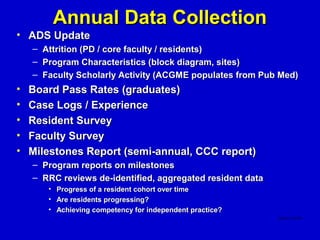
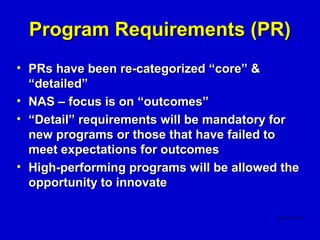
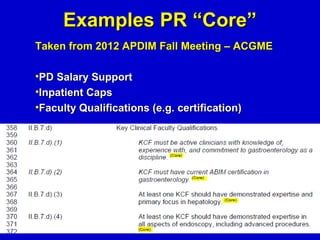
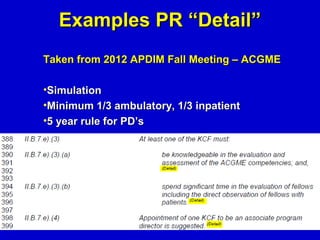
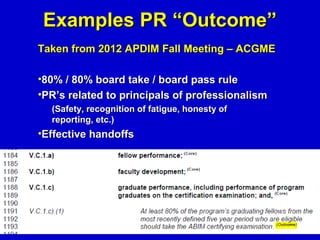
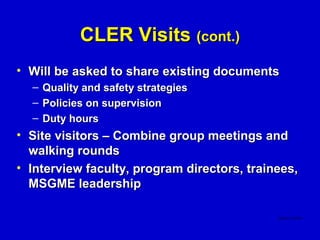
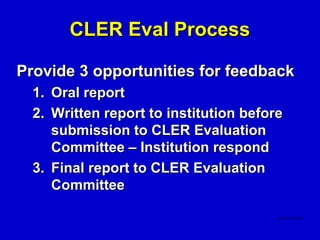
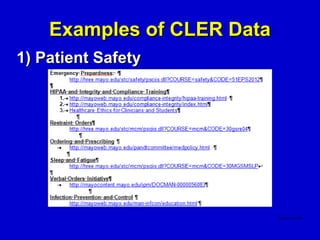
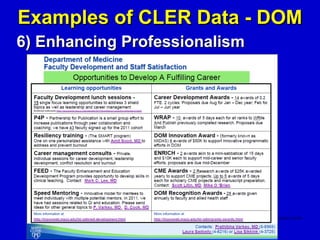
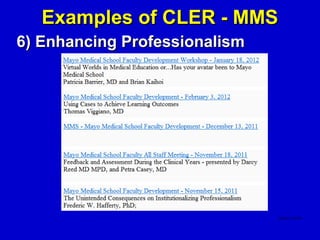
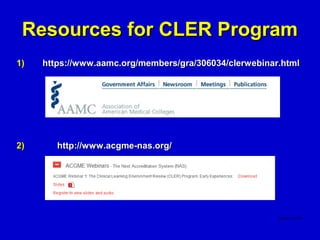
This document summarizes a presentation on the Next Accreditation System (NAS) for gastroenterology program coordinators. It discusses key aspects of NAS including the transition from process to outcomes-based accreditation, new requirements like the Clinical Learning Environment Review (CLER) program and milestones, and timelines for implementation. Details are provided on how requirements have been re-categorized as core, detailed, or outcomes and how programs will be evaluated annually through data collection, surveys, and site visits every 10 years with formative feedback.