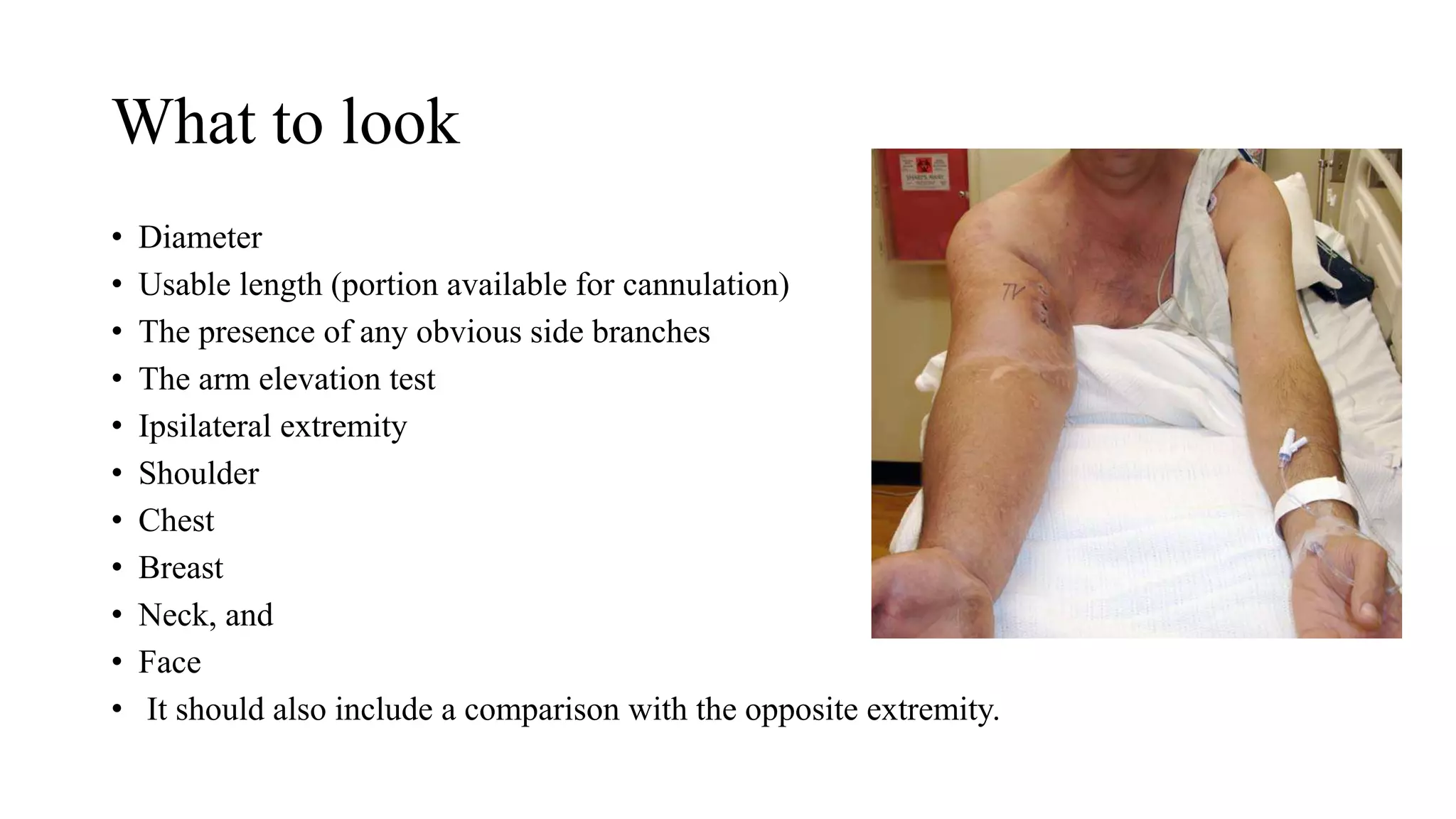
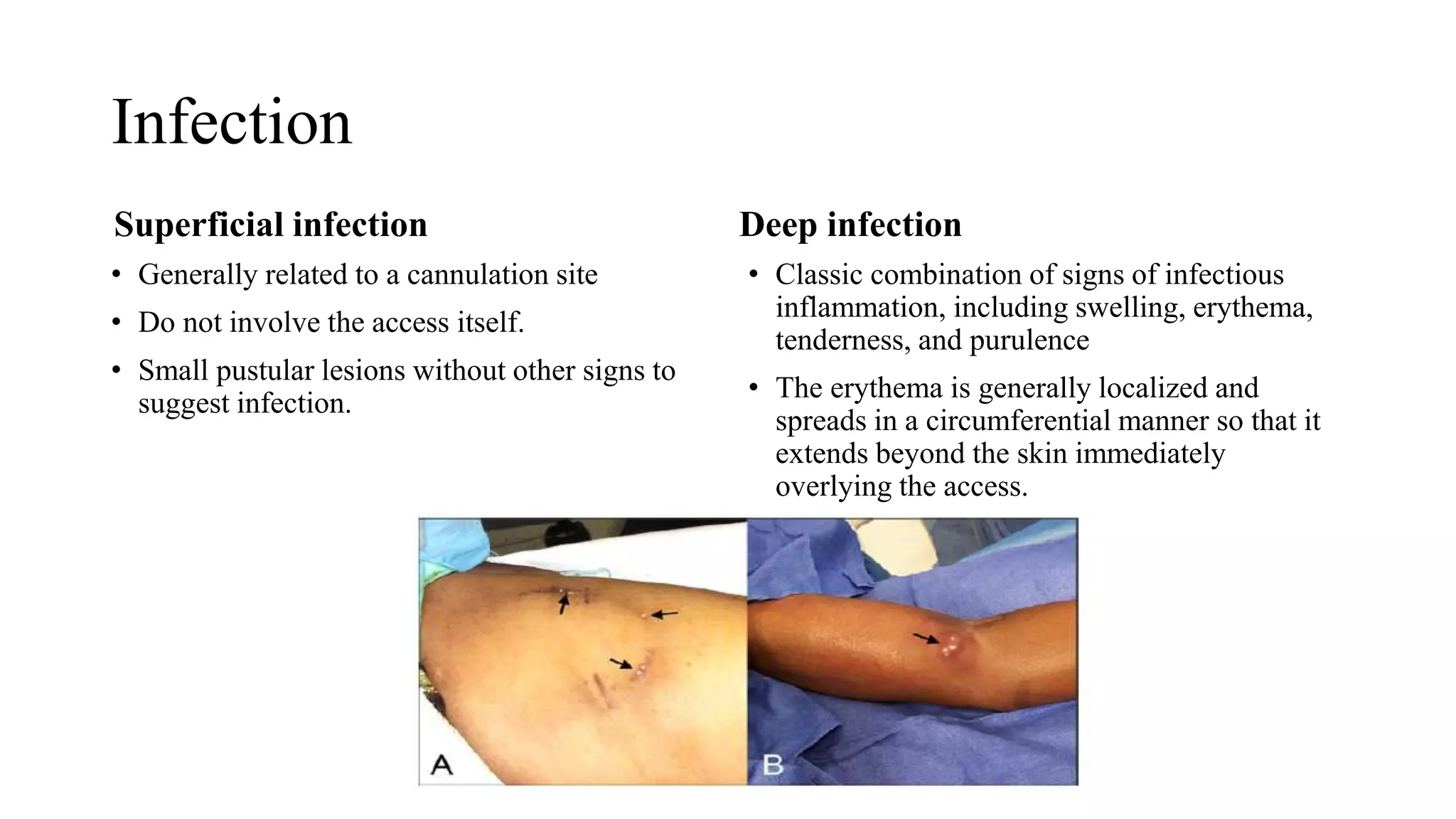
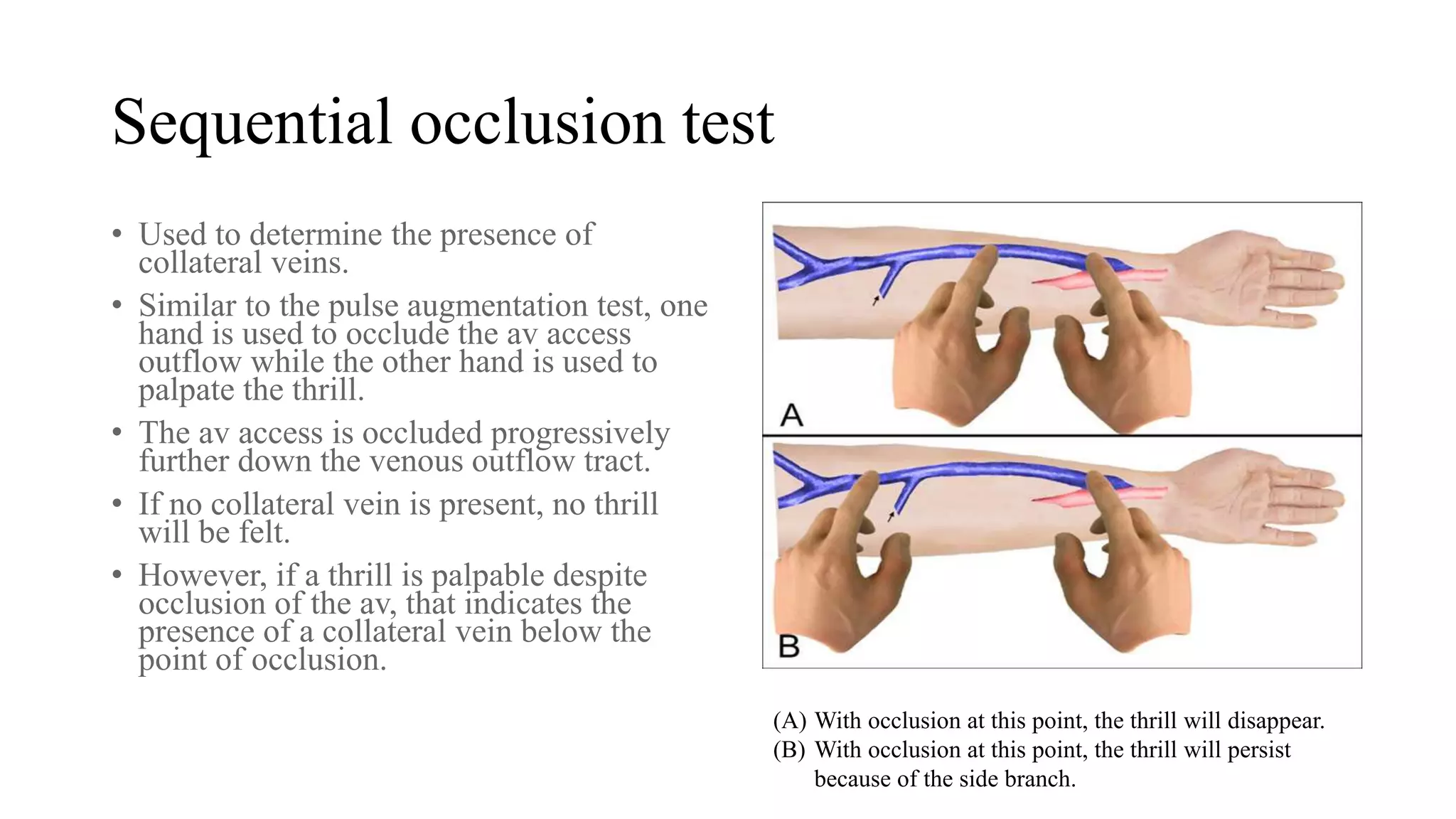
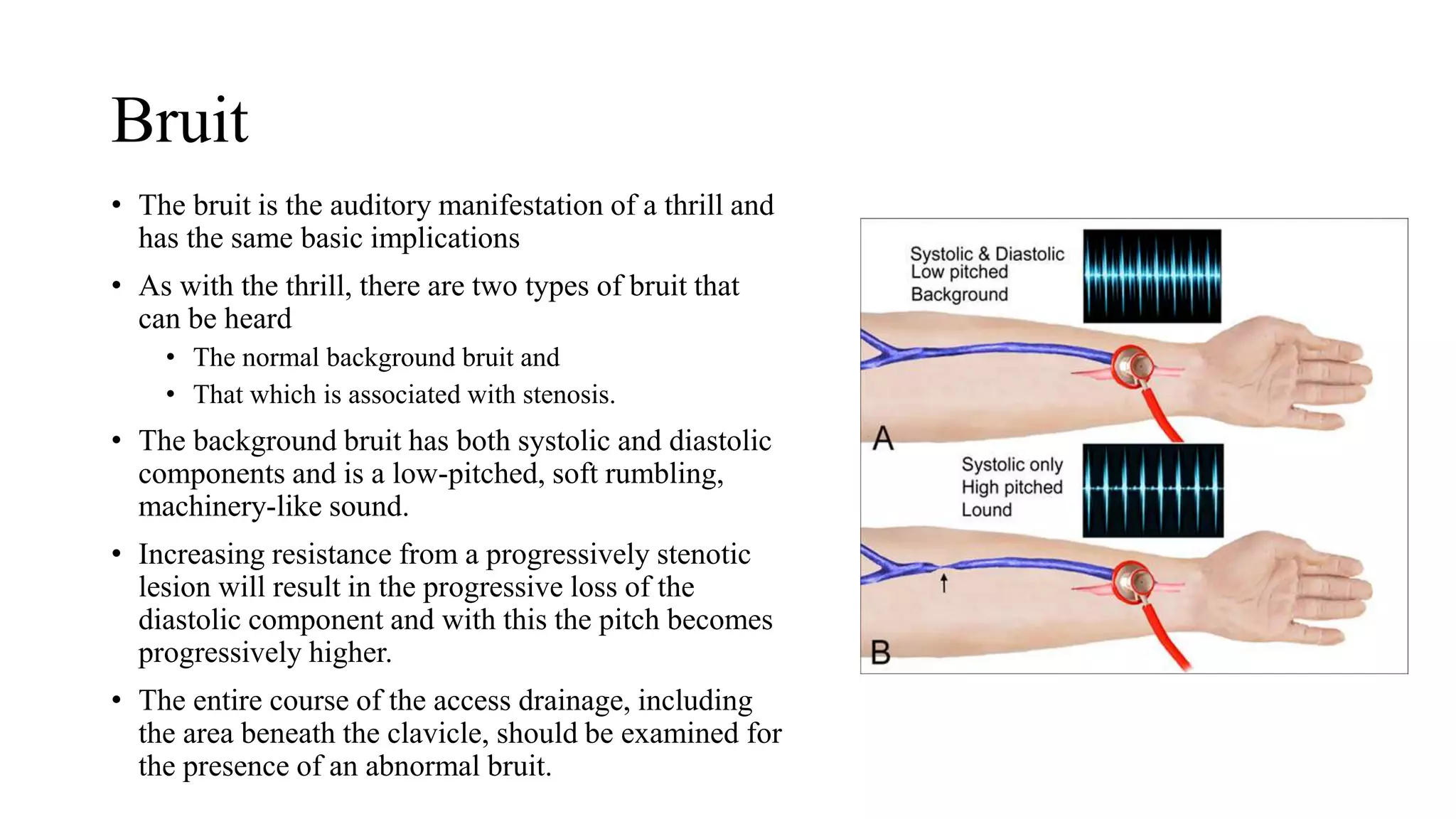
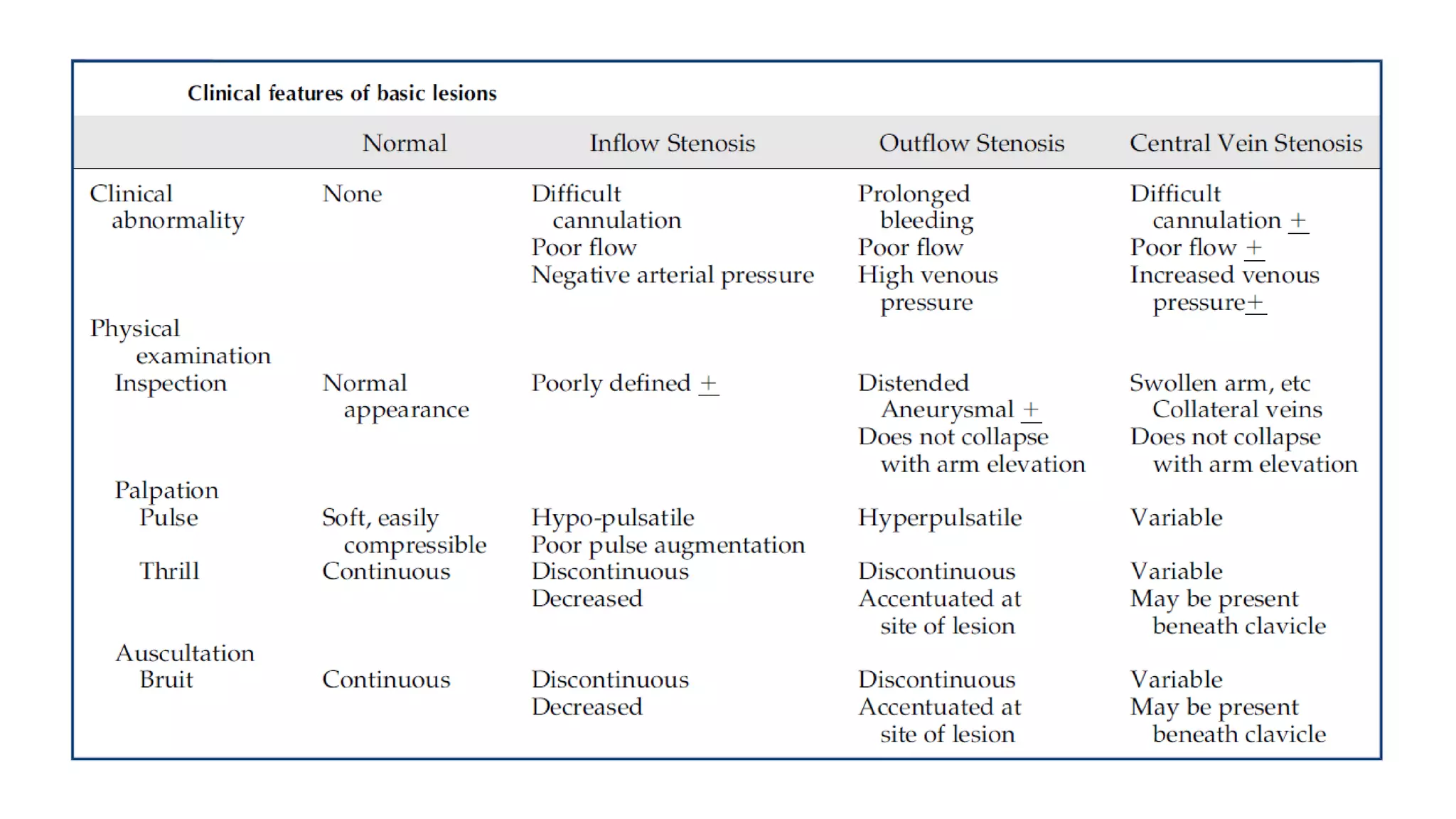
The document provides guidelines for regularly examining arterio-venous (AV) vascular access sites at least monthly through physical inspection, palpation, and auscultation to detect abnormalities. Examination can identify stenosis or other issues that may impair function without additional equipment costs. Inspection assesses access diameter, length, branches, and skin. Palpation feels for pulse, thrill, and uses occlusion tests. Auscultation listens for bruits indicating flow. Abnormal physical findings can indicate stenosis requiring intervention to maintain access patency.